Picture this: It’s a typical morning. You wake up feeling sluggish, check your blood sugar, and see a number higher than expected—again. Frustration builds as you wonder why your efforts aren’t paying off. If you’re living with diabetes, you’re not alone in facing these unexpected spikes or dips. Millions manage the condition daily, yet subtle habits can quietly undermine progress.
Research shows that small, everyday choices often separate stable control from ongoing struggles. The good news? Recognizing and sidestepping common pitfalls can make a real difference in how you feel and your long-term health outlook. Studies from sources like the Mayo Clinic and American Diabetes Association highlight how avoiding these errors supports steadier levels and fewer complications.
Curious which habits trip up even the most dedicated people? Let’s count them down—starting from number 8. Each one includes real-world scenarios and practical shifts. By the end, you’ll have tools to tighten your routine.
Mistake #8: Inconsistent or Infrequent Blood Sugar Monitoring
Meet Sarah, a 58-year-old office manager with type 2 diabetes. She tested sporadically, convinced her “good days” meant she could skip checks. Then came unexplained fatigue and higher A1C results that surprised her doctor.

Regular monitoring provides crucial feedback. The CDC notes that consistent checks help spot patterns early, allowing timely adjustments. Skipping tests—especially before/after meals or exercise—misses opportunities to catch highs or lows.
You might think, “My levels feel fine.” But silent fluctuations happen. Start small: set phone reminders for key times. Track trends in a simple app or notebook. The insight gained often motivates better choices.
But wait—monitoring is only part of the picture. What about the tools themselves?
Mistake #7: Using Expired or Improperly Stored Testing Supplies
John, 62, stretched his test strips to save money, using ones past expiration. His readings varied wildly, leading to confusion and unnecessary worry.
Expired strips or improperly stored insulin (too hot, frozen, or exposed to light) can give inaccurate results. WebMD reports that heat or cold degrades effectiveness, skewing data you rely on.
Always check dates and store supplies as directed—cool, dry place for strips; refrigerator for unopened insulin, room temp for in-use (avoid extremes). Replace lancets regularly for comfort and accuracy.
Feel that relief from reliable numbers? Yet, even perfect readings won’t help without the right fuel…
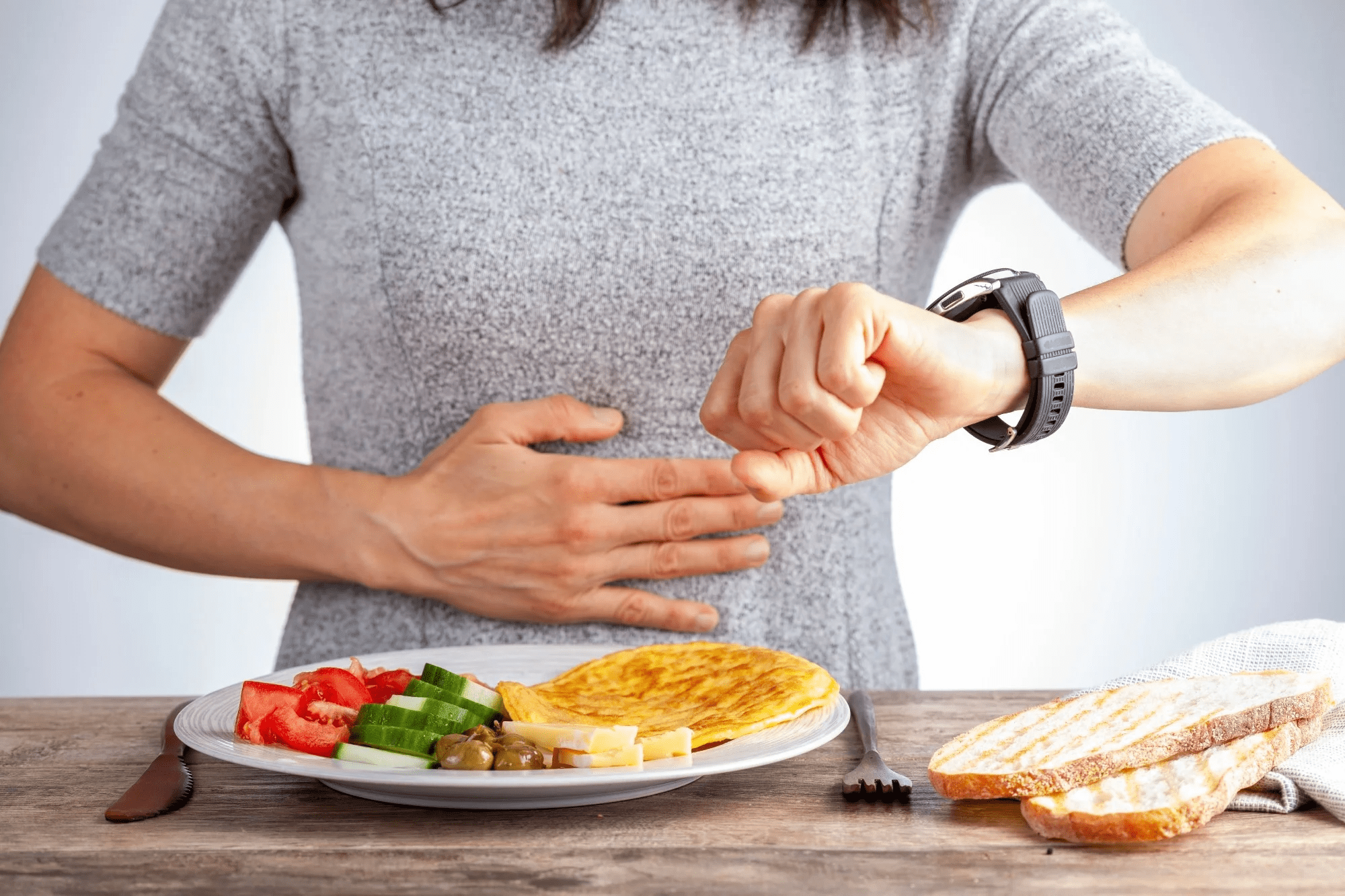
Mistake #6: Skipping Meals or Eating at Irregular Times
Imagine rushing through your day, skipping lunch, then crashing with low energy—or overeating dinner to compensate, sending levels soaring.
Skipping meals disrupts balance, especially if on insulin or certain meds. Mayo Clinic explains irregular timing can cause swings: lows from missed food, highs from compensatory overeating.
Aim for consistent meal timing. Include balanced options with protein, fiber, and healthy fats to stabilize energy. If busy, prep grab-and-go choices like Greek yogurt with nuts.
Intrigued how food choices amplify this? The next habit sneaks in unnoticed…
Mistake #5: Overlooking Hidden Carbs and Portion Sizes
Lisa, 55, avoided obvious sweets but loaded up on “healthy” granola bars and fruit juice, puzzled by persistent highs.
Many underestimate carbs in seemingly innocent foods—sauces, yogurt, bread. Portion creep adds up fast. The American Diabetes Association stresses carb awareness for steady control.
Read labels, use measuring tools initially, and try the plate method: half non-starchy veggies, quarter protein, quarter carbs. Small swaps—like whole fruit over juice—make big impacts.
You may wonder about drinks. That’s where the next mistake hits hard…
Mistake #4: Choosing Sugary or Dehydrating Beverages
Think of grabbing a soda or sweetened coffee to perk up. It tastes great momentarily, but spikes follow.
Sugary drinks cause rapid rises; even some “diet” options affect some people. Dehydration worsens control—diabetes already increases fluid loss risk.
Opt for water, unsweetened tea, or infused options (lemon, cucumber). Black coffee or green tea in moderation often works well. Hydration supports kidney function and clearer thinking.
Refreshing change, right? But movement matters too—yet many fall short here.
Mistake #3: Leading a Sedentary Lifestyle or Skipping Regular Activity

Tom, 60, knew exercise helped but let work and fatigue win. Weeks without movement led to creeping weights and stubborn levels.
Inactivity reduces insulin sensitivity. Regular activity—walking, strength training—improves how your body uses glucose. Mayo Clinic recommends at least 150 minutes weekly, plus breaking up sitting.
Start where you are: 10-minute walks after meals lower post-meal spikes. Build gradually. Consistency trumps intensity.
Statistic to ponder: Active people often see better A1C. But what about the one habit linked to faster complications?
Mistake #2: Smoking or Ignoring Other Heart Risks
Smoking narrows vessels, worsens circulation, and raises complication risks like heart disease, stroke, and poor healing.
The CDC and Mayo Clinic warn smoking compounds diabetes dangers—higher chance of nerve/kidney/eye issues. Quitting brings benefits quickly: better circulation, easier control.
If you smoke, talk to your provider about support—patches, counseling, meds. Manage blood pressure and cholesterol too; they’re intertwined.
Powerful shift ahead—the final mistake often surprises people…
Mistake #1: Inconsistent Medication Adherence or Timing
Around 60% don’t take meds exactly as prescribed, per WebMD experts. Skipping, doubling, or wrong timing disrupts balance.
Medications work best consistently. For insulin, timing with meals matters. Oral meds have windows too.
Use pill organizers, alarms, or link to routines (breakfast, bedtime). Discuss barriers with your doctor—adjustments possible.
This tops the list because it directly affects levels daily. Small habit tweaks yield compounding wins.
Quick Comparison: Common Mistakes vs. Smarter Alternatives
| Mistake Habit | Potential Impact | Smarter Alternative |
|---|---|---|
| Infrequent monitoring | Missed patterns, delayed fixes | Set routine checks + log trends |
| Expired/wrong storage supplies | Inaccurate readings | Check dates, proper storage |
| Skipping/irregular meals | Swings in levels | Consistent timing + balanced plates |
| Hidden carbs/poor portions | Unexpected highs | Label reading + portion awareness |
| Sugary/dehydrating drinks | Rapid spikes + dehydration | Water, unsweetened options |
| Sedentary routine | Reduced sensitivity | Daily movement + break sitting |
| Smoking/ignoring risks | Accelerated complications | Quit support + BP/cholesterol checks |
| Inconsistent meds | Unstable control | Reminders + doctor discussions |
Safe Steps to Break These Habits Today
Start with one or two changes—overhauling everything overwhelms. Track progress weekly. Many notice steadier energy within weeks.
Address doubts: “I’ve tried before.” Progress compounds; small wins build momentum. Partner with your healthcare team for tailored tweaks—adjustments based on your unique needs.
- Prioritize hydration and movement first for quick wins.
- Build a support network—friends, apps, or groups.
- Celebrate non-scale victories like better daily feel.
Take Control: Your Diabetes Journey Starts with Awareness
Imagine fewer surprises, more steady days, and confidence in your routine. Avoiding these habits isn’t about perfection—it’s empowerment.
You deserve to feel your best. Start today with one shift.
P.S. Did you know post-meal walks can drop levels noticeably? Try it after dinner for an easy boost.
Share in the comments: Which habit resonates most? Your story might help someone else.
This article is for informational purposes only and is not a substitute for professional medical advice—consult your healthcare provider for personalized guidance.