Picture this: You’re in your mid-50s, feeling the usual aches of a busy life, but something feels off during your morning routine. A subtle change in urination catches your attention. Could it be nothing—or the start of something serious? Prostate cancer often sneaks up without fanfare, but catching it early can shift everything. Imagine reclaiming your energy, your confidence, and your peace of mind with a straightforward check. We’ll explore the subtle clues, smart screening steps, and why acting now matters. Ready to take control? Let’s start with what you might be overlooking.
The Silent Threat: Why Prostate Cancer Often Hides in Plain Sight
Prostate cancer tops the list of common cancers for men, yet it rarely announces itself early on. About 85% of cases get spotted through routine checks, not symptoms. Think about it: Over 300,000 U.S. men face diagnosis yearly, but early detection boosts survival rates to near 100% for localized cases. Ignoring it? That’s like driving with a blindfold—risky and unnecessary. But here’s the hook: What if a quick blood test could reveal hidden risks before trouble brews? Keep reading; the signs might surprise you.
Many men chalk up changes to “just getting older.” Yet, unchecked, this cancer can spread quietly. Studies show delays in screening lead to advanced stages in up to 20% of cases. You’re not alone if you’ve skipped that doctor’s chat. Ever wonder if family stories hint at your own risk? Let’s uncover those next.
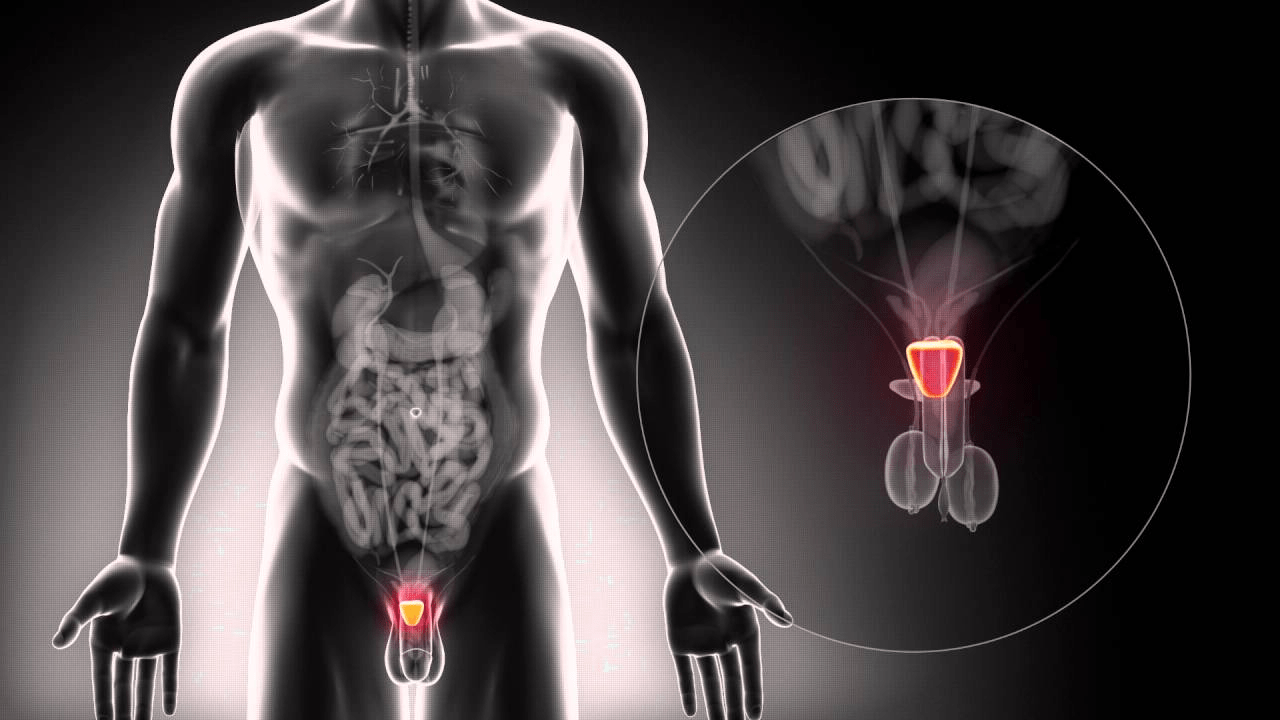
Know Your Risk: Factors That Raise the Odds
Age is the biggest red flag—risk jumps after 50, peaking at 65. If you’re African American, your odds double, with more aggressive forms possible. Family history? A father or brother with it ups your chance two- to threefold. Imagine Bob, 58, brushing off his dad’s early diagnosis as coincidence. Months later, a routine check saves him from progression. Sound familiar? Up to 60% of cases tie to genetics. But wait—lifestyle plays in too. Obesity links to faster-growing types. Could your habits be stacking the deck? The good news: Awareness is your first shield.
Top Risk Factors at a Glance
- Age Over 50: Most diagnoses hit here; risk triples by 60.
- Race/Ethnicity: Higher for Black men; discuss screening at 45.
- Family Ties: One close relative? Double risk. Two? Start checks at 40.
- Genetics: BRCA mutations or Lynch syndrome elevate odds—ask about testing.
- Lifestyle: High dairy/meat intake or excess weight may nudge risks up.
Spotting these early? It could mean years of hassle-free living. But symptoms—do they even show up?
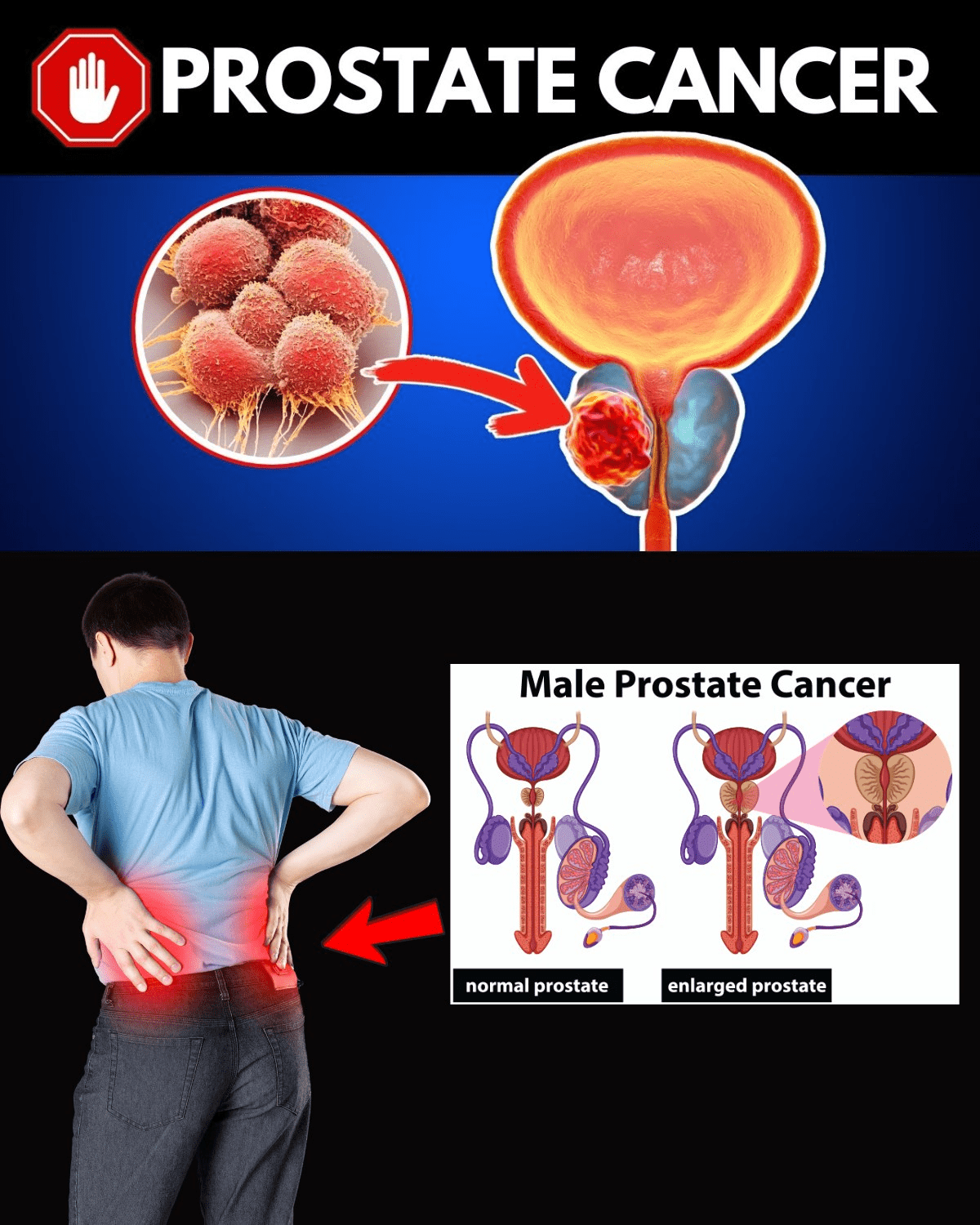
Subtle Symptoms: What to Watch For (Even If Rare)
Early prostate cancer whispers, not shouts. Most men feel fine until later stages. Still, tuning into your body pays off. Frequent nighttime bathroom trips? A weak stream? These hit 70% of men over 50, but rarely signal cancer alone. Blood in urine or semen? That’s a wake-up—see a doc ASAP, as it flags issues in 10-20% of cases. Ever pause mid-day, wondering if that pelvic ache is normal? You’re not imagining it; persistent discomfort warrants a look.
Meet Tom, 62, who ignored burning during urination as “prostate blues.” Turns out, it was early-stage cancer caught via follow-up. Relief washed over him like cool water after a hot day. Pain in hips or back? Advanced signs, but catching precursors early changes the game. You might think, “It’s probably nothing.” Fair, but why risk it? Next up: The tools that catch it first.
Common Early Clues (Often Overlooked)
- Difficulty starting or stopping urine flow.
- Needing to urinate more often, especially at night.
- Blood traces in urine or semen—don’t ignore this one.
- Erectile changes or ejaculation discomfort.
- Unexplained pelvic or lower back pain.
These mimic benign issues like enlargement, but checking rules out worries. Intrigued by foolproof detection? Let’s dive in.
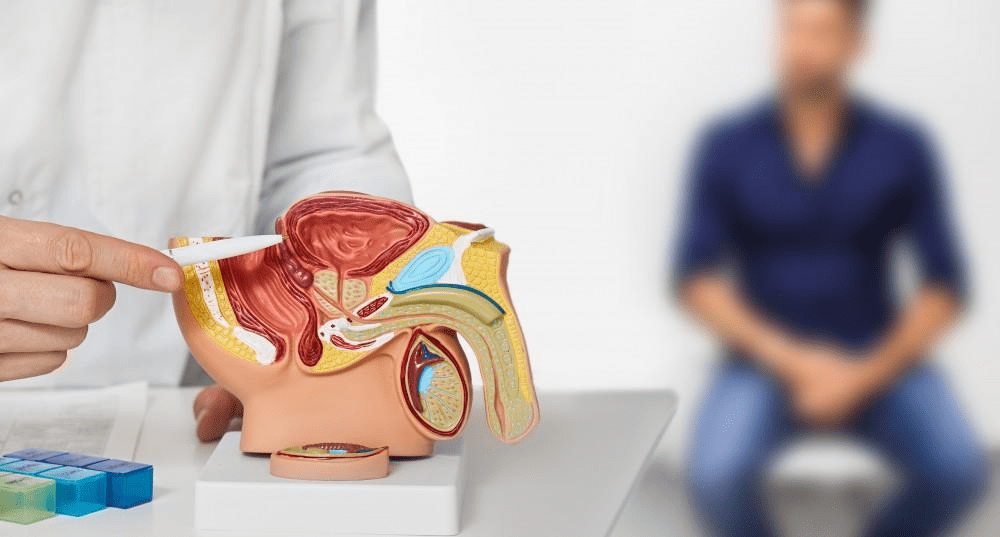
Screening Smarts: The Key to Early Wins
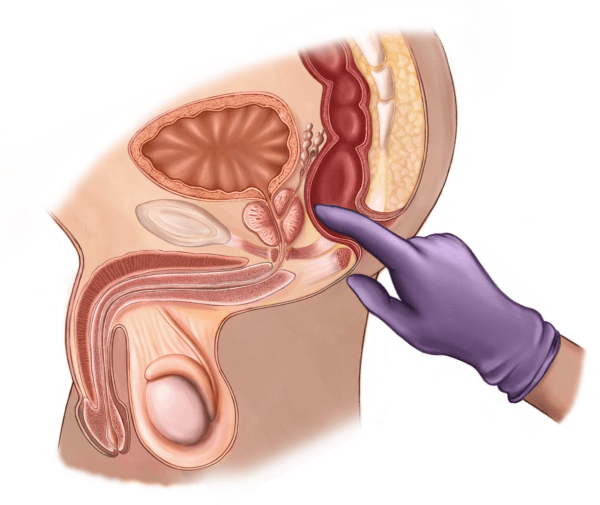
Screening isn’t one-size-fits-all—it’s a conversation. USPSTF says men 55-69 should weigh PSA testing with their doc. Why? It spots 80% of early cancers via a simple blood draw. PSA measures prostate-specific antigen; levels over 4 ng/mL often prompt deeper looks. Add a digital rectal exam (DRE)—a quick feel for lumps—and you’ve got a dynamic duo. Picture the relief: A normal result means more golf swings, fewer what-ifs.
For high-risk folks, start at 45 or 40. AUA guidelines push shared decisions, factoring family history. But hold on—over-screening can lead to unnecessary biopsies. Balance is key. Ever asked your doc about your baseline? It’s easier than you think.
| Screening Basics: PSA vs. DRE |
|---|
| Test |
| PSA Blood Test |
| DRE Exam |
Talk it out—your doc tailors it to you. But what if screening flags something?
Next Steps: From Suspicion to Confirmation
Elevated PSA? Don’t panic—it’s a clue, not a verdict. Next: Multiparametric MRI for detailed images, reducing false alarms by 30%. Then, biopsy—tiny samples checked for cancer cells. Sarah’s husband, 55, faced this after a routine PSA spike. The earthy scent of the clinic lingered, but clear results brought back his stride. Early findings mean options like active surveillance for slow-growers.
You might worry: “Biopsies hurt?” Mild discomfort, usually, with local numbing. Staging follows—scans check spread. Knowledge empowers; uncertainty drains. Ready to lower your risks further?
Lifestyle Tweaks: Boost Your Defenses Naturally
Can’t change age or genes? Fine—focus on what you can. Exercise cuts aggressive cancer risk by 30%. Aim for 150 minutes weekly; feel that post-walk glow? Tomatoes and veggies pack lycopene, potentially slashing odds 20%. Ditch excess dairy—studies link high intake to higher risks. John’s story: Swapping burgers for salads post-50 kept his PSA steady. Small shifts, big payoffs.
Quick Wins for Risk Reduction
- Walk briskly 30 minutes daily—builds resilience.
- Load plates with cruciferous veggies like broccoli.
- Maintain a healthy weight; shed pounds gradually.
- Limit red meat; opt for fish twice weekly.
- Stay hydrated—supports prostate health.
These aren’t cures, but they stack odds in your favor. Feeling empowered? One chat could seal it.
Your Action Plan: Talk, Test, Thrive
Start simple: Book that doc visit. Discuss risks, family history, and PSA timing. For average risk, baseline at 55; high-risk, sooner. Track changes—journal symptoms if any. Remember Tom and Bob? Their stories echo: Early action meant thriving, not surviving.
| Safe Screening Guide |
|---|
| Age Group |
| 40-54 (High Risk) |
| 55-69 (Average) |
| 70+ |
Consult always—personalized beats generic. You might think, “Too busy?” One hour now saves years later.
Seize the Day: Early Detection Saves Lives
Why wait for warning bells when you can ring them yourself? Spotting prostate cancer early unlocks 99% survival, smoother digestion, and vitality for grandkids’ games. You’ve got the risks, signs, and steps—now act. Schedule that screening; share this with a buddy. Empower yourself today. P.S. Fun fact: Regular checkups cut advanced diagnoses by 40%—your move counts.
This article is for informational purposes only and not a substitute for professional medical advice—consult your healthcare provider for personalized guidance.