Imagine going about your day when a dull, persistent pressure builds in your lower abdomen—like a heavy weight settling in that you can’t quite shake off. Or perhaps you notice your periods have become unpredictably heavier, soaking through protection faster than before, leaving you exhausted and anxious. Your uterus, that pear-shaped powerhouse of the female reproductive system, rarely complains loudly at first. Yet subtle changes can signal issues like fibroids, adenomyosis, endometriosis, prolapse, or even early uterine cancer.
These conditions affect millions of women, often overlapping in symptoms that are easy to dismiss as “normal” aging, stress, or hormonal shifts. Research from sources like the Mayo Clinic and Cleveland Clinic shows many women delay seeking care because signs feel vague or intermittent. What if tuning in early could bring relief and prevent bigger challenges? Let’s count down 12 common warning signs that your uterus may need attention—starting with the most frequently overlooked.
Sign 12: Unusual Vaginal Discharge That’s Different from Normal
You step out of the shower and notice a watery, pink-tinged, or foul-smelling discharge that lingers. It feels off, unlike your usual cycle.
This can stem from endometrial changes or infections. Studies link persistent unusual discharge to conditions like adenomyosis or early uterine concerns. You might think it’s minor—but patterns matter. But wait, the next sign disrupts daily life even more.
Sign 11: Painful Intercourse (Dyspareunia)

Picture intimacy turning uncomfortable—a sharp or deep ache during or after that leaves you hesitant. Many describe it as pressure or burning.
Common in endometriosis, adenomyosis, or fibroids pressing on tissues. Patient stories highlight how it strains relationships before women connect the dots. Ever wondered if it’s “just you”? It often isn’t.
Sign 10: Frequent Urination or Urgency
You find yourself rushing to the bathroom more often, even at night, with a constant “gotta go” feeling.
Fibroids or prolapse can press on the bladder. Data shows this as a key clue in pelvic floor issues. Imagine reclaiming uninterrupted nights—it’s possible with awareness.
Sign 9: Constipation or Bowel Changes
Straining during bowel movements or feeling incomplete emptying becomes routine. Some notice rectal pressure.
This ties to posterior prolapse or fibroids affecting nearby organs. Many overlook it until it worsens. But the following sign hits closer to home.
Sign 8: Lower Back or Pelvic Pressure That Lingers
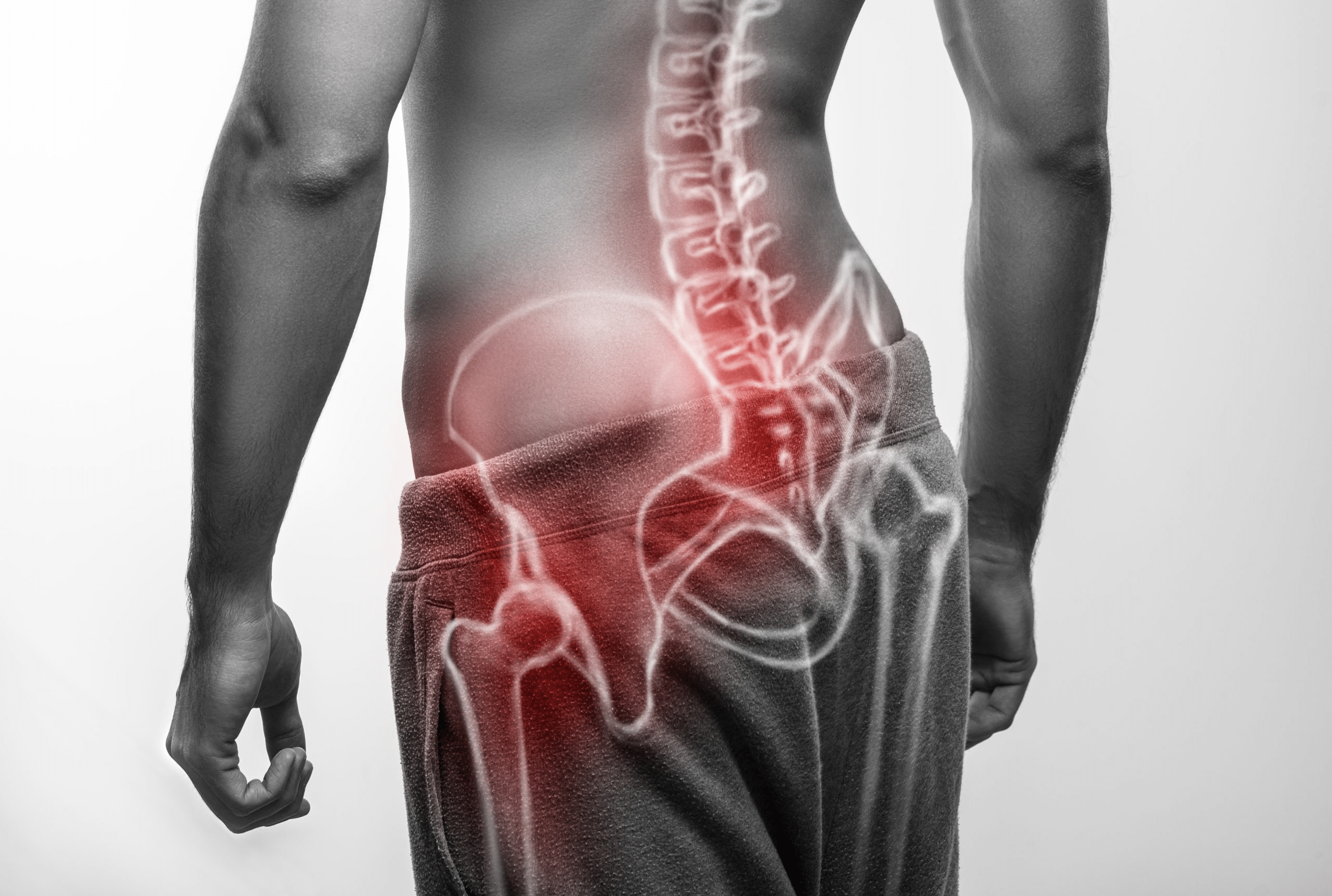
A constant ache in your lower back or a “fullness” in the pelvis, like something’s weighing you down after standing.
Often linked to enlarged uterus from fibroids or adenomyosis. Research notes this subtle pressure builds gradually. You might blame posture—but it could be more.
Sign 7: Enlarged or Bloated Abdomen (“Adenomyosis Belly”)
Your lower belly protrudes noticeably, mimicking early pregnancy even without weight gain.
Heavy fibroids or adenomyosis can double or triple uterine size. Women report feeling self-conscious about the change. Intrigued? The next ones involve your cycle.
Sign 6: Bleeding Between Periods (Spotting)
Unexpected light bleeding or spotting mid-cycle disrupts your routine.
This flags abnormal uterine bleeding from polyps, fibroids, or precancerous changes. It’s often brushed off as irregular hormones.
Sign 5: Heavy or Prolonged Periods (Menorrhagia)
Periods so heavy they soak pads/tampons hourly, lasting over 7 days, or with large clots.
A hallmark of fibroids, adenomyosis, and sometimes endometrial issues. Many experience fatigue from blood loss. But hold on—these can escalate.
Sign 4: Severe Menstrual Cramps (Dysmenorrhea)

Cramps that double you over, unresponsive to usual pain relief, radiating to thighs.
Common in endometriosis and adenomyosis. Stories describe missing work or social plans. You might think it’s normal—but intensity matters.
Sign 3: Pain or Pressure in the Pelvis Outside Periods
Ongoing dull ache or sharp twinges in the pelvic area, unrelated to your cycle.
This signals chronic conditions like endometriosis or growing fibroids. Research ties it to inflammation and pressure.
Sign 2: Feeling of Something Bulging or Falling Out
A sensation like a tampon is slipping out, or visible bulge at the vaginal opening, especially after standing long.
Classic for uterine prolapse or pelvic floor weakness. Many feel embarrassed but find relief knowing it’s common.
Sign 1: Postmenopausal Bleeding or Any Bleeding After Menopause
Any spotting, light bleeding, or discharge after 12 months without periods.
This is the most critical red flag for uterine cancer, per CDC and American Cancer Society guidelines. Early detection dramatically improves outcomes. Like many women who hesitated, getting checked brought answers and peace.
Here’s a quick comparison of these signs and common associated conditions:
| Sign | Often Linked To | Why It Matters |
|---|---|---|
| Unusual Discharge | Adenomyosis, Endometrial Changes | Can indicate cellular shifts |
| Painful Intercourse | Endometriosis, Fibroids | Affects intimacy and quality of life |
| Frequent Urination | Fibroids, Prolapse | Signals organ pressure |
| Constipation/Bowel Issues | Posterior Prolapse | Overlaps with daily comfort |
| Lower Back/Pelvic Pressure | Enlarged Uterus (Fibroids/Adenomyosis) | Subtle but persistent |
| Enlarged Abdomen | Adenomyosis, Large Fibroids | Visible change in body shape |
| Bleeding Between Periods | Polyps, Fibroids | Abnormal uterine bleeding |
| Heavy/Prolonged Periods | Fibroids, Adenomyosis | Leads to anemia and fatigue |
| Severe Cramps | Endometriosis, Adenomyosis | Disrupts daily activities |
| Chronic Pelvic Pain | Multiple Conditions | Indicates ongoing inflammation |
| Bulging Sensation | Uterine Prolapse | Direct pelvic floor sign |
| Postmenopausal Bleeding | Uterine Cancer (Key Alert) | Urgent evaluation needed |
These patterns often overlap—many women have more than one condition.
For safe next steps, follow this guide:
| Action Step | How to Proceed | Safety Notes |
|---|---|---|
| Track Symptoms | Journal bleeding, pain, and patterns | Note duration, intensity, triggers |
| Schedule Pelvic Exam | See gynecologist for routine check | Includes ultrasound if needed |
| Discuss Family History | Mention relatives with similar issues | Helps assess risk factors |
| Consider Lifestyle Support | Pelvic floor exercises (Kegels), weight management | Gentle ways to strengthen support |
| Seek Prompt Care | For postmenopausal bleeding or severe pain | Don’t wait—early checks matter |
You might be thinking, “Is this really serious?” Many signs stem from benign issues like fibroids, yet patterns warrant checking. Women like those sharing stories of ignored heavy bleeding later found treatable causes—empowering them with options.
Three key takeaways: Never ignore postmenopausal bleeding, track changes in your cycle and pain, and prioritize pelvic health discussions with your doctor.
Take one step today—note any recent changes and book that appointment. Your body speaks quietly at first; listening early can make all the difference.
P.S. Did you know pelvic floor exercises can ease mild prolapse symptoms for many? Start simple and build strength!
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.