Imagine waking up to a subtle, nagging discomfort that you brush off as just another busy day. You’re in your mid-40s, juggling work and family, when a faint, unusual scent lingers after your morning routine. It feels off, but life pulls you forward. What if that whisper from your body is trying to alert you to something serious? In this article, we’ll uncover nine early signs of cervical cancer that many women overlook, blending real stories with insights to help you stay informed. Picture the relief of catching a potential issue early—it’s like turning on a light in a dim room. But first, let’s explore why these signs often slip under the radar.
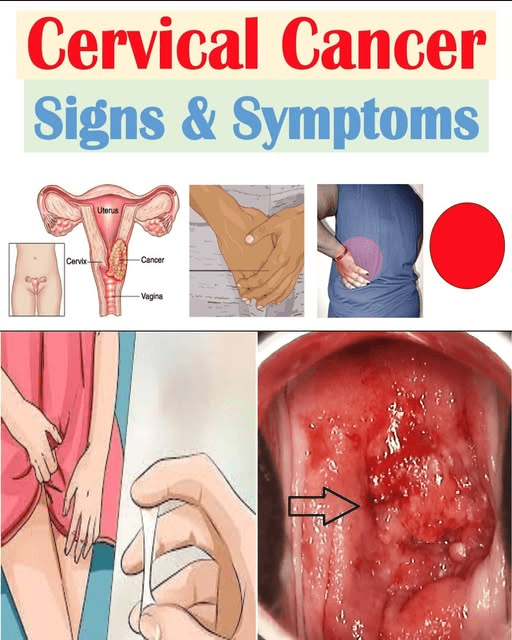
Cervical cancer can sneak up quietly, affecting thousands of women each year. According to health organizations, over 14,000 new cases are diagnosed annually in the U.S., yet early detection could change outcomes dramatically. The problem? Many dismiss early symptoms as normal aging or stress.
These overlooked signs lead to delayed care, turning minor concerns into bigger challenges. Women often feel isolated, wondering if they’re overreacting. Have you ever ignored a twinge because it seemed too vague?
But what if recognizing these signals could empower you? Let’s build suspense as we count down the nine signs, starting with the subtle ones. Each could be a clue your body is sending—stay tuned for the first.
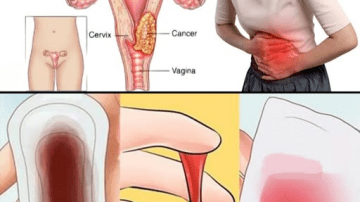
Sign 9: Unusual Vaginal Discharge That Feels Different
Sarah, a 48-year-old teacher from Chicago, noticed a watery discharge with a faint, fishy odor during her evening shower. At first, she thought it was just hormonal fluctuations from perimenopause. But as weeks passed, the sticky texture persisted, leaving her feeling uneasy and distracted.
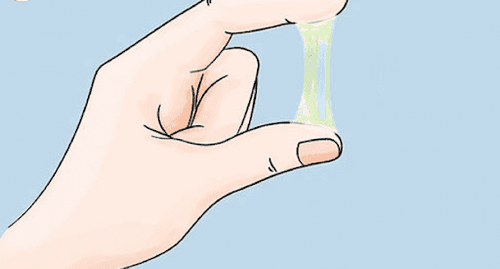
Research suggests that changes in discharge—becoming watery, bloody-tinged, or foul-smelling—may indicate cellular shifts in the cervix. Studies from the American Cancer Society highlight how infections or precancerous cells could trigger this. Yet, many women attribute it to everyday causes.
You might be thinking, “Isn’t this common?” True, but persistent changes warrant attention. Imagine the peace from a simple check-up. But hold on, the next sign might surprise you even more.
Sign 8: Pain or Discomfort During Intimacy
Picture Lisa, 52, from New York, who felt a sharp sting during a romantic evening, like sandpaper against sensitive skin. She dismissed it as dryness from aging, but the recurring ache left her anxious about closeness.
Evidence from medical journals shows that cervical issues can cause friction or bleeding during sex, potentially linked to inflammation or growths. A study in the Journal of Women’s Health noted this in early-stage cases.
What if this isn’t just “getting older”? It could be your body’s way of signaling help. Addressing it early might restore comfort. But wait, there’s a sign that’s even sneakier ahead.
Sign 7: Abnormal Bleeding Between Periods
One afternoon, Emily, 46, from Texas, spotted unexpected blood on her underwear, a metallic scent hitting her as she changed. She chalked it up to stress from her job, but the irregular spotting kept interrupting her routine.

Data from the CDC indicates that bleeding outside cycles or after menopause may stem from cervical abnormalities. Research involving thousands of women links this to HPV-related changes.
Ever wondered why your body sends mixed signals? It might be urging awareness. Spotting this could lead to timely insights. And the countdown continues with a persistent ache.
Sign 6: Persistent Pelvic Pain That Lingers
John’s wife, Maria, 50, from California, described a dull throb in her lower abdomen, like a heavy weight pressing down after a long walk. She ignored it, assuming it was from her yoga class, but the constant pressure affected her sleep.
Clinical reviews suggest ongoing pelvic discomfort could relate to cervical pressure on nearby tissues. A report from Mayo Clinic connects this to advancing cellular changes.
But you might think, “It’s probably nothing serious.” Sometimes it is—listening early offers clarity. Imagine feeling lighter. Yet, the next sign hides in plain sight.
Sign 5: Unexplained Fatigue That Drains Your Energy
Recall Anna, 47, from Florida, who felt exhausted by midday, her coffee tasting bitter as she pushed through errands. She blamed it on poor sleep, but the bone-deep tiredness made simple tasks feel monumental.
Studies in oncology journals point to how the body fighting early cancer cells might cause this overwhelming weariness. Fatigue often accompanies immune responses, per research from the National Cancer Institute.
Is this just life catching up? It could be more. Recognizing it might recharge your days. But don’t stop—the following sign sneaks up unexpectedly.
Sign 4: Sudden Weight Loss Without Trying
Tom noticed his partner, Rebecca, 49, from Seattle, shedding pounds effortlessly, her clothes hanging loose with a faint musty smell from skipped meals. She felt thrilled at first, but the unexplained drop worried her friends.

Health experts note that metabolic shifts from cervical issues may lead to appetite loss or nutrient absorption problems. A study in The Lancet observed this in early detections.
You might say, “Who wouldn’t want that?” But it signals imbalance. Catching it could balance your health. And now, a sign that radiates outward.
Sign 3: Lower Back Pain That Won’t Quit
In her quiet moments, Sophia, 51, from Boston, rubbed her aching lower back, feeling a warm, throbbing pulse after sitting too long. She thought it was from gardening, but the pain radiated like a persistent echo.
Medical literature ties chronic back discomfort to cervical cancer spreading to nearby structures. Research from Harvard Medical School links this to nerve involvement.
Ever dismissed backaches as routine? They might whisper deeper truths. Addressing them could ease your load. But hold your breath—the next is visible.
Sign 2: Swelling in the Legs or Feet
David’s aunt, Laura, 53, from Atlanta, noticed her ankles puffing up by evening, the skin tight and shiny under her socks. She attributed it to standing all day at work, but the swelling persisted even on rest days.
Experts explain that lymphatic blockages from cervical growths can cause edema. A clinical trial reported in the British Journal of Cancer found this in advanced early cases.
What if it’s not just poor circulation? It could be a call to action. Spotting it early might prevent escalation. And finally, the top sign that changes everything.
Sign 1: Urinary Problems Like Frequent Urges
Meet Karen, a 45-year-old nurse from Denver, who experienced sudden urges to urinate, accompanied by a burning sensation that disrupted her shifts. At first, she linked it to too much caffeine, but the frequency left her frustrated and fatigued. Before recognizing it as a potential sign, Karen felt overwhelmed and isolated. After consulting her doctor, she gained clarity and relief through early screening—transforming her anxiety into empowerment.
Scientific insights reveal that cervical pressure on the bladder may cause incontinence or infections. The World Health Organization’s data shows this as a key indicator in many diagnoses.
But you might wonder, “Isn’t this typical for women my age?” Often yes, but persistence suggests checking. This sign could truly shift your health trajectory.
To wrap these signs, here’s a quick comparison to help differentiate them from everyday issues:
| Sign | Common Cause | Potential Cervical Link |
|---|---|---|
| Unusual Discharge | Hormones or infections | Cellular changes causing odor or tint |
| Pain During Intimacy | Dryness from age | Inflammation or growths |
| Abnormal Bleeding | Stress or cycles | HPV-related abnormalities |
| Pelvic Pain | Exercise strain | Tissue pressure |
| Fatigue | Poor sleep | Immune response |
| Weight Loss | Diet changes | Metabolic shifts |
| Lower Back Pain | Posture issues | Nerve involvement |
| Leg Swelling | Standing long | Lymphatic blockage |
| Urinary Problems | Caffeine intake | Bladder compression |
This table highlights how signs overlap with normal life—yet patterns matter.
Now, for safe steps forward, consider this guide:
| Action Step | How to Proceed | Safety Notes |
|---|---|---|
| Self-Monitor | Track symptoms in a journal | Note duration and triggers; don’t self-diagnose |
| Schedule Check-Up | See a gynecologist annually | Discuss family history; Pap tests may help detect early |
| Lifestyle Adjustments | Maintain healthy weight, avoid smoking | These can reduce risks, per studies |
| Seek Support | Join women’s health forums | Emotional backing aids, but consult pros |
| Emergency Signs | Heavy bleeding or severe pain | Visit ER immediately; better safe |
Remember, these are potential steps—always personalize with a healthcare provider.
You might be thinking, “What if I’m overreacting?” Many women feel that way, like Sarah and Karen in our stories. They hesitated but found empowerment through action. Research shows early awareness can lead to better discussions with doctors.
But that’s not all—imagine missing these whispers and regretting it later. By spotting them, you gain control. Three key takeaways: Listen to unusual discharge, heed intimacy discomfort, and track bleeding patterns.
Empower yourself today—schedule that check-up. What small step will you take? As a P.S., did you know regular HPV vaccines, even in adulthood, might offer protection? Share this with a friend—it could spark a vital conversation.
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.