Picture this: You’re going about your day, noticing a small change—like spotting between periods or a slight discomfort during intimacy—and you think, “It’s probably nothing. Maybe stress, hormones, or just getting older.” Many women dismiss these subtle signals, assuming they’re harmless or temporary. But what if those quiet clues are early whispers from your body about something more serious?
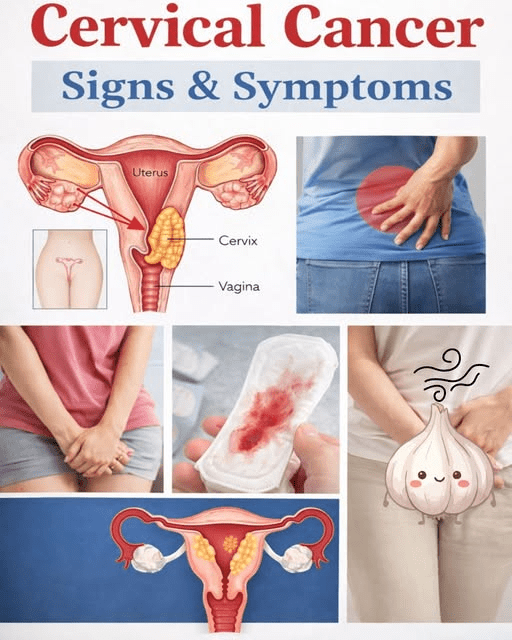
Cervical cancer often develops slowly, starting from changes caused by persistent HPV infection. In its earliest stages, it frequently produces no noticeable symptoms at all—that’s why regular screenings like Pap tests and HPV tests remain the gold standard for catching it before it advances. Yet when signs do appear, they can be easy to overlook or attribute to other common issues like infections, fibroids, or menopause.
Millions of women worldwide face this disease, but early awareness and prompt medical attention dramatically improve outcomes. You’re about to explore nine early warning signs that research and experts from sources like Mayo Clinic, American Cancer Society, and others say women frequently miss or downplay.
Why These Signs Are Often Overlooked
Early cervical cancer tends to be silent because the cervix lacks many pain-sensitive nerves. Symptoms usually emerge only when the disease progresses slightly or affects nearby tissues.
Many women hesitate to discuss vaginal changes, bleeding, or discomfort due to embarrassment or the belief it’s “normal.” But these patterns deserve attention—especially if they persist, worsen, or appear without clear cause.
Let’s count down nine key signs, starting with those most commonly brushed aside.
Sign 9: Unexplained Fatigue or Low Energy
You feel unusually tired despite resting well, or everyday tasks drain you more than before.
While fatigue links to many conditions (stress, anemia, thyroid issues), advanced cervical cancer can cause it through blood loss or the body’s response to the disease. Some women notice this creeping exhaustion early on.
If tiredness pairs with other changes, it’s worth mentioning to your doctor.
Sign 8: Frequent or Urgent Urination Changes
You find yourself needing the bathroom more often, feeling urgency, or experiencing discomfort while urinating.
These urinary shifts can signal the cancer pressing on the bladder or ureters. Early involvement might cause subtle irritation or frequency that feels like a mild UTI—but doesn’t resolve with typical treatment.
Don’t assume it’s always a simple infection.
Sign 7: Lower Back, Pelvic, or Abdominal Discomfort
A dull ache in your lower back, pelvis, or abdomen lingers without injury or obvious reason.
Persistent pelvic pressure or pain—sometimes described as a heavy feeling—can occur as the tumor grows or irritates surrounding tissues. Many attribute it to menstrual cramps, ovulation, or aging.
If it doesn’t ease with usual remedies, get it checked.
Sign 6: Pain or Discomfort During Intercourse
Sex feels uncomfortable, painful, or causes spotting afterward.
Dyspareunia (painful intercourse) or post-coital bleeding ranks among the more specific early clues. Friction against a fragile cervix can cause bleeding or soreness that women might blame on dryness, infection, or position.
This sign often prompts women to finally seek care.
Sign 5: Unusual Vaginal Discharge Changes
Your discharge looks, smells, or feels different—thicker, watery, pink-tinged, bloody, or foul-smelling.
Watery, bloody, or odorous discharge that persists differs from normal variations. Many dismiss it as a yeast or bacterial issue, but when linked to cervical changes, it can signal abnormal cells or early invasion.
Track any ongoing shift.
Sign 4: Heavier, Longer, or More Irregular Periods
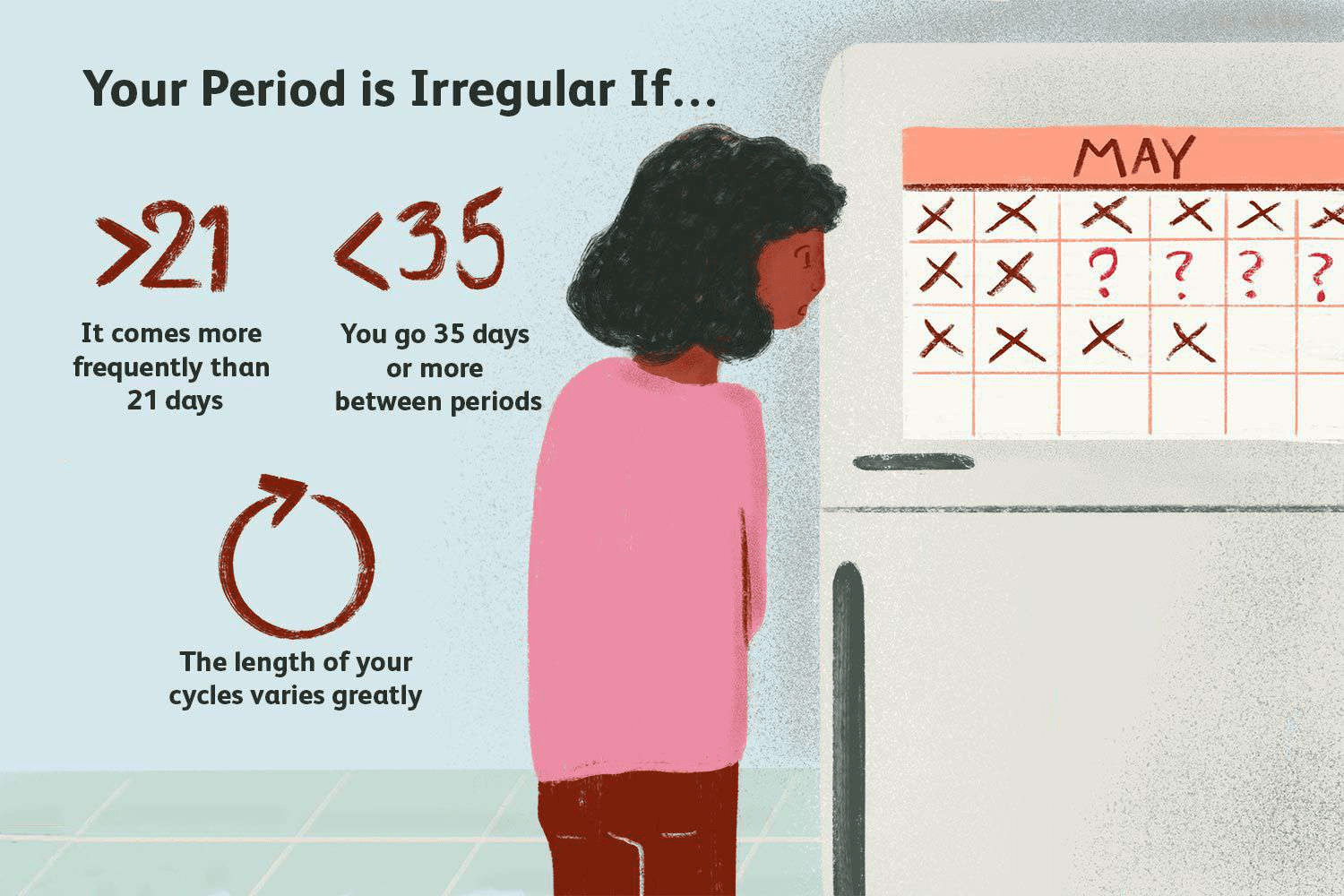
Menstrual bleeding suddenly becomes heavier, lasts longer, or feels more intense than your norm.
This change can stem from the cervix bleeding more easily. Women often attribute it to perimenopause, stress, or birth control—but unexplained shifts warrant evaluation.
Sign 3: Bleeding Between Periods or After Menopause
Spotting or light bleeding occurs mid-cycle, after sex, douching, or—critically—after menopause.
Postmenopausal bleeding is never normal and ranks as one of the strongest red flags. Between-period spotting or bleeding after intercourse often gets overlooked as “irregular cycles” or minor irritation.
Experts call this one of the most common yet missed early indicators.
Sign 2: Spotting or Bleeding After Intercourse
Even light contact causes spotting or bleeding afterward.
This postcoital bleeding happens because fragile, abnormal cervical tissue bleeds easily. Many women feel embarrassed or assume it’s from roughness, but recurring episodes signal the need for prompt screening.
Sign 1: Abnormal Vaginal Bleeding Overall (The Most Commonly Noticed Yet Delayed)
Any vaginal bleeding that’s unusual for you—between periods, after sex, heavier than normal, or after menopause—stands out as the top symptom women eventually report.
Sources like Mayo Clinic, American Cancer Society, and oncologists emphasize that abnormal bleeding prompts most diagnoses. Yet women often wait weeks or months before mentioning it, hoping it resolves on its own.
This delay can allow progression—making early reporting crucial.
Patterns to Watch For
These signs often appear in combination rather than alone. They may start subtly and worsen gradually.
Early cervical cancer is highly detectable and treatable through routine Pap/HPV screening—many cases never progress to symptomatic stages when caught early.
You might wonder: “Is every unusual symptom cancer?” No—most vaginal changes stem from benign causes like infections, polyps, or hormonal shifts. But persistence or multiple signs together deserve professional evaluation.
Why Acting Early Makes a Difference
Cervical cancer remains one of the most preventable cancers thanks to vaccination against HPV and regular screenings. When found early, treatment success rates soar.
If any of these resonate—even mildly—don’t wait. Schedule a visit with your gynecologist or primary care provider. Simple tests can provide clarity and peace of mind.
Three key takeaways:
- Abnormal vaginal bleeding (any kind) tops the list of symptoms women notice but often delay reporting.
- Subtle changes like unusual discharge, pain during sex, or pelvic discomfort frequently get overlooked.
- Routine screenings remain the best defense—many early cases show no symptoms until caught on tests.
Your body speaks in whispers before it shouts. Listening early empowers you.
P.S. Keeping a simple symptom journal (dates, descriptions) helps when discussing concerns with your doctor.
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.