Have you ever noticed unexplained brown spots on your shins that won’t fade? Or felt a patch of skin on your neck that suddenly looks darker and feels velvety? These subtle skin changes are easy to ignore or blame on aging, dryness, or sun exposure. But for many people, they serve as quiet signals that blood sugar levels might be out of balance—potentially pointing to diabetes or prediabetes.
Diabetes affects how your body processes glucose, and high levels over time can impact blood vessels, nerves, and skin health. According to sources like the American Academy of Dermatology, American Diabetes Association, and Cleveland Clinic, skin issues appear in up to 30-70% of people with diabetes at some point, and sometimes they show up before other classic symptoms like thirst or frequent urination.
In this article, we’ll count down 8 key skin signs commonly linked to diabetes. These can stem from many causes—only a healthcare professional can diagnose the underlying issue. If you spot persistent changes, especially multiple ones, see your doctor promptly for evaluation, which may include blood sugar testing.
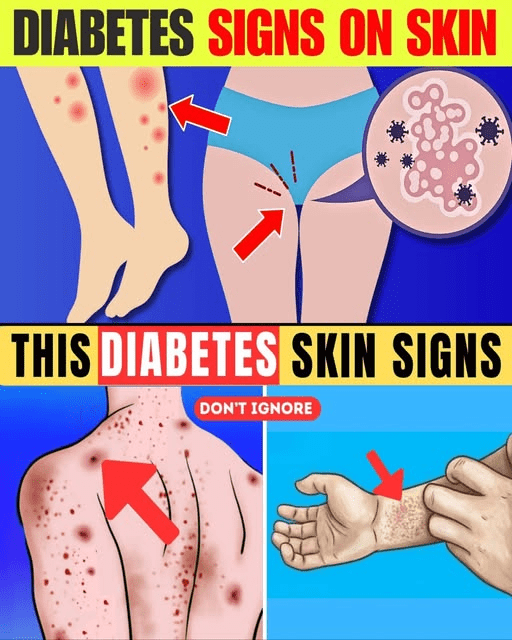
Here are some clear visuals to help recognize common diabetes-related skin changes:
Now, let’s explore the countdown—starting from number 8.
Sign 8: Frequent or Slow-Healing Infections

Hot, red, swollen areas or recurring fungal/yeast rashes (often in moist folds like underarms or groin) that linger longer than usual.
High blood sugar can weaken your immune response and feed yeast or bacteria. These infections might itch, burn, or ooze, and take weeks to clear instead of days.
Sign 7: Dry, Itchy Skin That Doesn’t Improve
Persistent dryness, scaling, or intense itching, even with moisturizers.
Elevated glucose draws fluid from tissues, leaving skin dehydrated. Cracks can form, raising infection risk—especially on legs and feet.
Sign 6: Eruptive Xanthomatosis (Sudden Yellow Bumps)
Small, firm, yellow-red bumps that appear suddenly, often on arms, legs, buttocks, or hands.
These result from high triglycerides linked to uncontrolled diabetes. The bumps may itch and resemble pimples but cluster in groups.
Here’s a closer look at how these bumps might appear:
Sign 5: Diabetic Blisters (Bullosis Diabeticorum)

Sudden, painless blisters on hands, feet, legs, or forearms—no injury involved.
These rare blisters fill with clear fluid and heal on their own in weeks, often without scarring. They’re more common in long-standing diabetes with neuropathy.
Sign 4: Necrobiosis Lipoidica Diabeticorum (Shiny Patches)
Reddish-brown or yellowish patches, often on the shins, with a waxy center and visible blood vessels.
This condition starts as small spots that expand into shiny, atrophic areas. It may itch, hurt, or ulcerate if irritated—more common in women.
Check out these examples of the distinctive patches:
Sign 3: Acanthosis Nigricans (Dark, Velvety Patches)
Thickened, dark, velvety skin, usually on the neck, armpits, groin, or knuckles.
This classic sign often signals insulin resistance and prediabetes or type 2 diabetes. It’s especially common in people carrying extra weight.
Here are visuals of this velvety texture in common areas:
Sign 2: Bacterial or Fungal Skin Infections That Recur
Red, itchy, moist rashes (often Candida yeast) in skin folds, or boils and styes that keep coming back.
Diabetes creates a favorable environment for microbes. If infections return despite treatment, it may indicate rising blood sugar.

Sign 1: Diabetic Dermopathy (Shin Spots)
Light brown or reddish spots on the shins—round or oval, scaly at first, then flattening over time.
This harmless but common condition affects up to 50% of people with diabetes. It results from small blood vessel changes and is often an early clue.
See how these typical “shin spots” look on real skin:
But could these just be normal skin changes? In many cases, yes—dry skin, rashes, or spots can come from aging, allergies, or poor circulation. Diabetes-related signs tend to persist, worsen, or appear in clusters. Most are more noticeable when blood sugar is poorly controlled.
Consider Maria, a 52-year-old office worker who ignored dark neck patches and recurring yeast infections for years, thinking it was just “middle-age skin.” When shin spots appeared, she finally got checked—prediabetes was caught early, and lifestyle changes helped reverse some signs.
Or take David, 58, who noticed painless blisters on his feet. Quick evaluation revealed type 2 diabetes, allowing him to start management before complications grew.
These stories highlight why paying attention matters—early action often leads to better outcomes.
What Should You Do If You Notice These Signs?
Monitor changes for a few weeks: note location, duration, and any patterns. If spots spread, infections recur, or skin darkens persistently, see your primary doctor or dermatologist. They may check blood sugar (A1C or fasting glucose), examine the skin, or refer you for further tests.
Managing blood sugar through diet, exercise, and medication (if needed) can improve or prevent many of these skin issues.
Bottom line: Your skin often reflects what’s happening inside. Ignoring persistent changes could mean missing a chance for early intervention. Listen to your body—it’s worth checking.
P.S. Keeping skin moisturized and blood sugar stable can go a long way toward preventing these issues—small daily habits make a big difference.
This article is for informational purposes only and is not a substitute for professional medical advice. Skin changes can overlap with many other conditions. Readers are strongly encouraged to consult a healthcare provider for any concerning symptoms and receive personalized guidance. Early evaluation is key—your health is worth protecting.