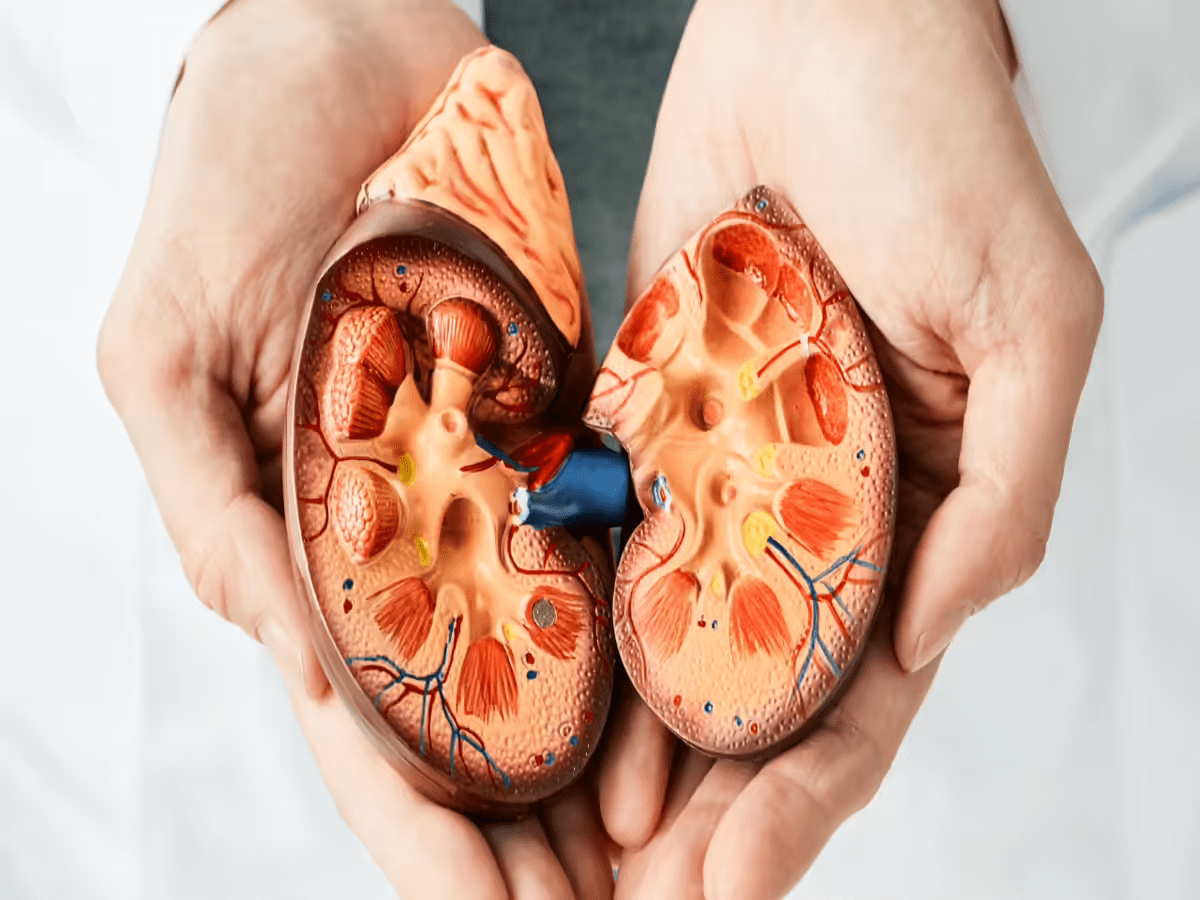
Imagine reaching for that familiar bottle of pain relievers after a long day, only to wonder if it’s quietly harming the organs that keep you going. Your kidneys filter waste, balance fluids, and regulate blood pressure—vital jobs that billions of microscopic nephrons handle every day. But certain everyday meds can disrupt this delicate process, potentially leading to reduced function or worse. What if the pills in your cabinet are putting extra strain on them? Studies suggest up to 20% of acute kidney injuries tie back to medications. If you’re over 50, managing chronic conditions, or just popping OTC drugs, this could hit close to home. Ready to uncover seven common culprits and how to sidestep trouble?
Why Medications Pose a Risk to Your Kidneys
Kidneys process about 200 liters of blood daily, but they’re sensitive to toxins, dehydration, and inflammation. Common meds can reduce blood flow, form damaging crystals, or inflame tissues, per research from the National Kidney Foundation. Ever skipped a doctor’s chat before starting a new pill? That’s when risks spike—especially if you’re dehydrated or have high blood pressure. The fallout? Fatigue, swelling, or even chronic issues. But knowledge is power. Curious which meds top the danger list?
7 Common Medications to Watch
These aren’t villains, but overuse or combos can tip the scales. Here’s a breakdown, backed by science. Always chat with your doctor before changes.
1. NSAIDs: The Pain Reliever Trap
Meet Linda, 58, who relied on ibuprofen for arthritis flares. One morning, she felt unusually swollen, her energy sapped. Tests revealed early kidney strain from years of daily doses. NSAIDs like ibuprofen (Advil) or naproxen (Aleve) block prostaglandins, easing pain but constricting kidney blood vessels. A 2022 study linked long-term use to a 25% higher chronic kidney disease risk. Feel that familiar ache? Alternatives like acetaminophen might help short-term. But wait—the next one’s hiding in your bathroom cabinet.
2. ACE Inhibitors: Blood Pressure’s Double Edge

Tom, 65, started lisinopril for hypertension and felt great at first. Then came the foamy urine and fatigue. These meds, like lisinopril (Prinivil) or enalapril (Vasotec), relax vessels to lower pressure but can drop kidney filtration if overdone. Research shows they may raise acute injury odds in dehydrated folks. Picture steady heartbeats without the worry—monitoring helps. Skeptical? The following med’s even more ubiquitous.
3. Diuretics: Water Pills That Dry You Out
Sarah, 62, took hydrochlorothiazide for swelling and loved the lighter feel. Until leg cramps hit hard. These “water pills” flush excess fluid but can dehydrate, starving kidneys of blood flow. A Mayo Clinic review notes heightened risks with other meds. Imagine relief without the thirst—stay hydrated. But hold on, antibiotics might be next on your radar.
4. Antibiotics: Infection Fighters with a Punch
John, 70, beat a UTI with ciprofloxacin, but follow-up labs showed creatinine spikes. Aminoglycosides like gentamicin or fluoroquinolones can form kidney crystals or inflame tubules. Up to 10% of hospital kidney injuries stem from these, per WebMD. That post-meal chill? It could mask bigger issues. Ever popped one casually? The next duo targets gut woes.
5. Proton Pump Inhibitors: Heartburn’s Hidden Cost
Emily, 55, swore by omeprazole for reflux, its chalky aftertaste a small price. Months later, persistent back pain signaled trouble. PPIs like omeprazole (Prilosec) cut stomach acid but may build up magnesium or inflame kidneys long-term. A Johns Hopkins study found 20-50% higher chronic disease risk. Soothe without the sting? Diet tweaks help. But the following one’s a cholesterol staple.
6. Statins: Cholesterol Control Caution
Robert, 68, managed lipids with atorvastatin, feeling empowered. Then swelling crept in. These lower bad cholesterol but can strain kidneys in high doses, especially with CKD. Evidence suggests worsened function in vulnerable groups. Visualize clear arteries, clear tests—regular checks matter. One more: the laxative lurking in drawers.
7. Laxatives: Quick Relief, Slow Burn
Maria, 60, used bisacodyl for constipation bouts, its bitter edge forgotten. Dehydration followed, taxing her kidneys. Stimulant types like senna deplete fluids, mimicking diuretic risks. Overuse ties to acute injury, notes AARP. Gentle fiber instead? It could change everything. See how they stack up?
How These Meds Compare in Risk
Each hits kidneys differently, but patterns emerge. Here’s a snapshot:
| Medication | Common Use | Potential Kidney Impact | Key Risk Factor |
|---|---|---|---|
| NSAIDs | Pain/inflammation | Reduced blood flow, inflammation | Long-term/high-dose use |
| ACE Inhibitors | High blood pressure | Dropped filtration rate | Dehydration combos |
| Diuretics | Swelling/hypertension | Dehydration, electrolyte imbalance | Low fluid intake |
| Antibiotics | Infections | Crystal formation, cell damage | High doses/short courses |
| PPIs | Heartburn/reflux | Magnesium buildup, chronic inflammation | Prolonged daily use |
| Statins | High cholesterol | Worsened function in CKD | Existing kidney issues |
| Laxatives | Constipation | Fluid loss, strain | Frequent reliance |
Intrigued by prevention? Let’s get practical.
Spotting the Signs Early
You might think, “I’m fine—no symptoms yet.” But kidneys whisper before they shout. Watch for swelling in ankles, foamy urine, or unexplained fatigue. A simple blood test tracks creatinine levels. Ever ignored a twinge? Early chats with docs catch it. But how do you use these safely?

Safe Use: Your Action Plan
Starting smart protects what matters. Here’s a guide:
| Medication | Safe Practices | Frequency Tip | When to Call Doc |
|---|---|---|---|
| NSAIDs | Lowest dose, shortest time; hydrate well | As needed, <10 days | Swelling or dark urine |
| ACE Inhibitors | Pair with monitoring; avoid if dehydrated | Daily as prescribed | Dizziness or creatinine rise |
| Diuretics | Drink extra water; eat potassium-rich foods | Daily with meals | Cramps or extreme thirst |
| Antibiotics | Finish course but report side effects | Short-term only | Reduced urine or rash |
| PPIs | Use for <8 weeks; try lifestyle first | Daily if needed | Persistent fatigue |
| Statins | Get regular kidney labs; watch interactions | Daily evening | Muscle pain or yellowing skin |
| Laxatives | Opt for fiber over stimulants; hydrate | Occasional | Ongoing constipation |
Consult pros before tweaks—especially with multiples. Linda switched to topicals and saw labs improve. You could too.
Protect Your Kidneys Starting Now
What if one unchecked pill leads to dialysis regrets? These seven—NSAIDs, ACE inhibitors, diuretics, antibiotics, PPIs, statins, laxatives—offer relief but demand respect. Research shows mindful use cuts risks dramatically. Empower yourself: review your meds yearly, stay hydrated, and prioritize whole foods. Your kidneys thank you with every balanced beat. Take charge today—book that check-up and sip water mindfully.
P.S. Did you know just 8 glasses of water daily can buffer med effects? Share this with a loved one on pills!
This article is for informational purposes only and not a substitute for professional medical advice. Consult your healthcare provider for personalized guidance.