Imagine a sudden, sharp stab in your lower left abdomen that makes you double over, accompanied by a fever that leaves you shivering. This isn’t just “stomach trouble”—it could be diverticulitis, a painful inflammation or infection of small pouches (diverticula) in your colon wall.
While many people have harmless diverticulosis (those pouches) without issues, when they become inflamed, it can escalate quickly. Research from Mayo Clinic and Cleveland Clinic shows that prompt attention prevents serious complications like abscesses, perforation, or even life-threatening infections. Have you felt unexplained abdominal discomfort lately? These six signs could be red flags—don’t brush them off. Let’s break them down so you can act fast if they appear.
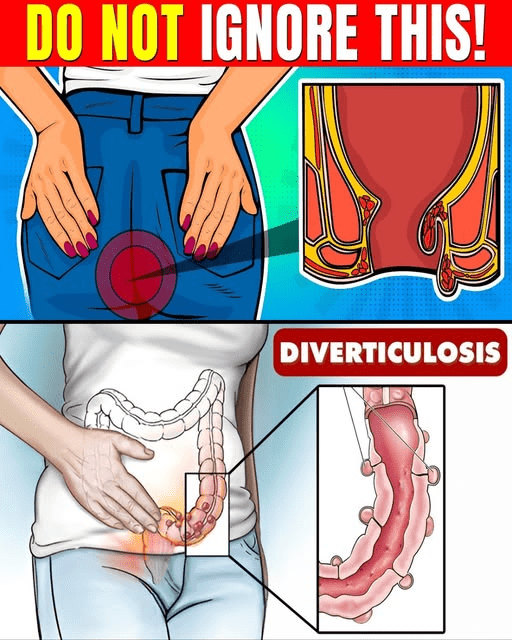
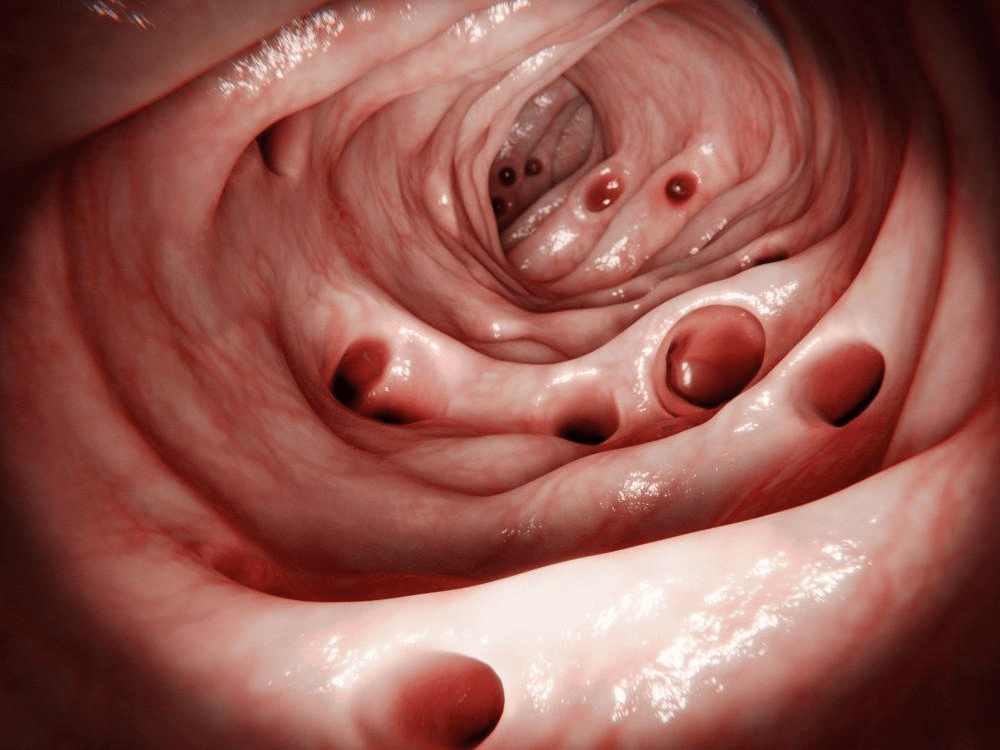
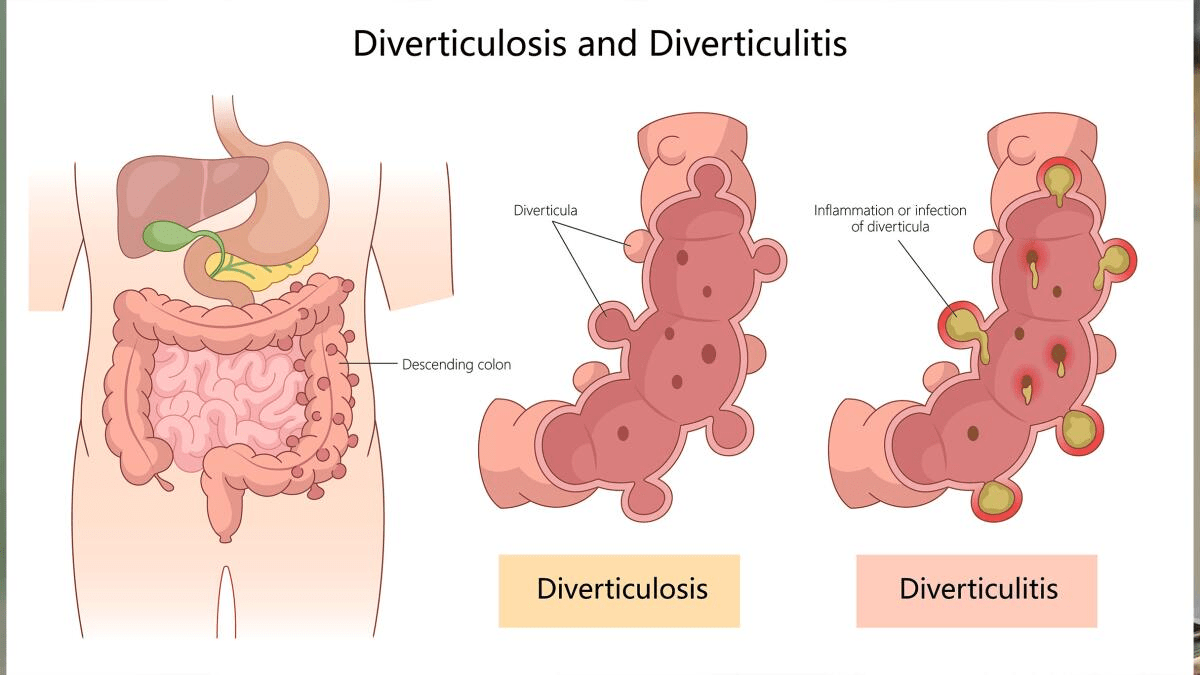
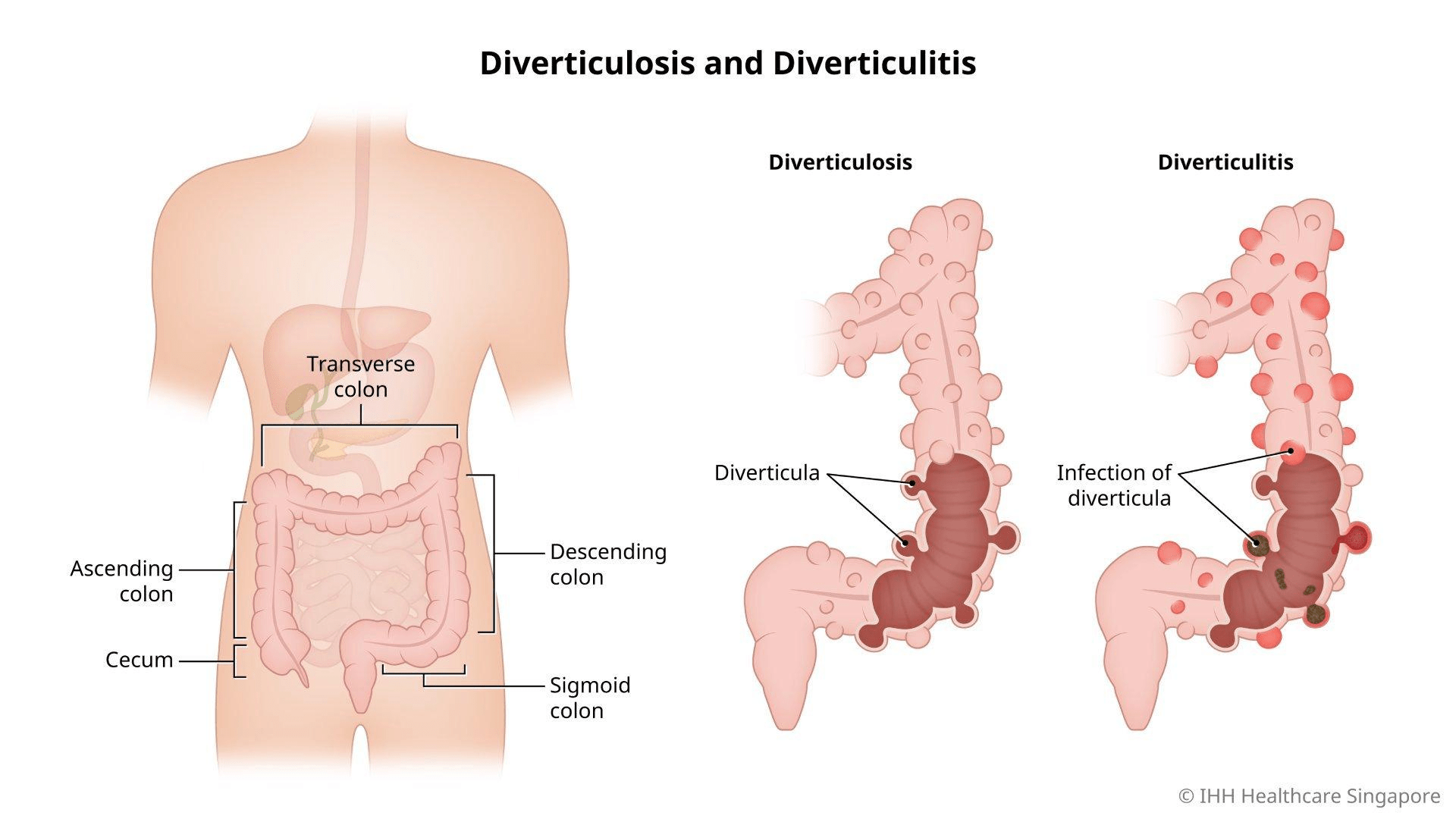
Here are some clear illustrations showing diverticulitis in the colon:
The Quiet Build-Up to a Painful Flare
Diverticulitis often strikes suddenly, especially in people over 50. A low-fiber diet may contribute to pouch formation, and when stool or bacteria get trapped, inflammation follows. Symptoms typically hit the lower left side, but can vary.
Mild cases might resolve with rest and diet, but ignoring key signs risks complications. Studies emphasize early recognition reduces hospital stays. What if that nagging pain signals something more?
Why These 6 Signs Are Emergency Red Flags
These symptoms often indicate active inflammation or infection. When combined, they raise the risk of perforation, abscess, or peritonitis. Mayo Clinic notes constant pain with fever demands quick evaluation. You might think, “It’s probably just gas”—but evidence shows better outcomes with timely care.
Here are the 6 signs you should never ignore:
Sign #6: Sudden Changes in Bowel Habits
Alternating constipation and diarrhea, or a sudden shift from normal patterns? This common sign reflects colon irritation.
Many report straining or loose stools during flares. It may seem minor, but paired with pain, it signals trouble. But hold on—the core symptom is far more intense.
Sign #5: Nausea and Vomiting
Feeling queasy or unable to keep food down? Inflammation disrupts digestion, leading to nausea.
Research links this to bowel blockage or irritation. Imagine the discomfort worsening—next comes fever.
Sign #4: Fever and Chills
A rising temperature, often with chills or sweating, points to infection.
Cleveland Clinic highlights fever as a key indicator of bacterial involvement. This systemic sign means your body fights inflammation—don’t wait.
Sign #3: Rectal Bleeding or Bloody Stools
Seeing bright red blood, maroon, or black tarry stools? This may indicate diverticular bleeding from eroded vessels.
While sometimes painless, it demands immediate checks. You might wonder if it’s hemorrhoids—but in context, it’s serious.
Here are diagrams highlighting common abdominal pain locations and affected areas:
Sign #2: Severe, Persistent Abdominal Tenderness
Pain that worsens with touch or movement, often sharp and localized to the lower left side.
Tenderness suggests inflammation spreading. Mayo Clinic urges urgent care if pain is constant and unexplained.
Sign #1: Severe Abdominal Pain with Systemic Symptoms
The top warning: Intense, sudden lower abdominal pain combined with fever, nausea, or vomiting.
This cluster often signals complicated diverticulitis. Many describe it as the worst pain they’ve felt—acting quickly can prevent perforation.
Here are the 6 key signs to watch:
- Sudden, severe lower left abdominal pain
- High fever and chills
- Nausea and vomiting
- Changes in bowel habits (constipation/diarrhea)
- Rectal bleeding or bloody stools
- Abdominal tenderness or distension
| Sign | Common Description | Why It’s Serious | When to Seek Emergency Care |
|---|---|---|---|
| Severe Abdominal Pain | Sharp, lower left side, worsening | May indicate perforation or abscess | If sudden/intense + fever |
| Fever & Chills | Temperature rise, shivering | Suggests active infection | With abdominal pain |
| Nausea/Vomiting | Persistent queasiness, inability to eat | Risk of dehydration/blockage | If unable to keep fluids down |
| Bowel Changes | Sudden constipation/diarrhea | Reflects colon irritation | Persistent + other symptoms |
| Rectal Bleeding | Bright red or dark blood in stool | Possible vessel rupture | Any noticeable blood |
| Tenderness/Distension | Pain on touch, bloated abdomen | Potential peritonitis | Rigid or highly sensitive abdomen |
What to Do If You Notice These Signs
Seek medical help promptly—don’t wait for symptoms to worsen. Your doctor may order a CT scan for confirmation.
- Track symptoms: Note pain location, fever, and bowel changes.
- Stay hydrated but avoid solid foods during acute flares (per guidance).
- Avoid self-treatment with NSAIDs—they may worsen bleeding risk.
You might think, “It’s probably nothing”—but many regret delaying. Early antibiotics or rest often resolve uncomplicated cases.
Protect Yourself—Don’t Wait for a Crisis
What if ignoring one sign leads to hospitalization? Recap: Severe pain, fever, nausea, bowel changes, bleeding, and tenderness—these could mean diverticulitis. Recognizing them empowers quick action.
Talk to your healthcare provider today if any resonate. Small awareness steps safeguard your gut health. P.S. Most flares improve with proper care—early detection makes all the difference!
Share your experiences below—your story might help others.
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.