Picture this: You’re going about your day, maybe noticing you’ve lost a few pounds without trying, or your back aches more than usual after meals. You shrug it off as stress, aging, or something minor. But what if these quiet changes are your body’s desperate signals for help? Pancreatic cancer is often called the “silent killer” because it hides so well—symptoms rarely appear until the disease has advanced. In 2026, estimates show about 67,500 new cases in the U.S. alone, with a five-year survival rate stuck at around 13%. Early awareness could make all the difference. Let’s dive into 12 critical warning signs that demand your attention—don’t ignore them.
Pancreatic cancer starts in the pancreas, the organ behind your stomach that helps with digestion and blood sugar control. Tumors often grow without causing obvious trouble early on. By the time symptoms emerge, the cancer may have spread. Reliable sources like the Mayo Clinic, Cleveland Clinic, and American Cancer Society stress that these signs are nonspecific—meaning they could stem from many causes—but when they persist or combine, they warrant prompt medical evaluation.
The urgency is real. Many people adapt to subtle changes until something alarming forces action. Have you felt unusually tired lately, or noticed changes in your digestion? These could be clues. Let’s count down 12 symptoms, starting with the more subtle ones and building to those that often signal advanced disease. Each one has shocked patients and families when they finally connected the dots.
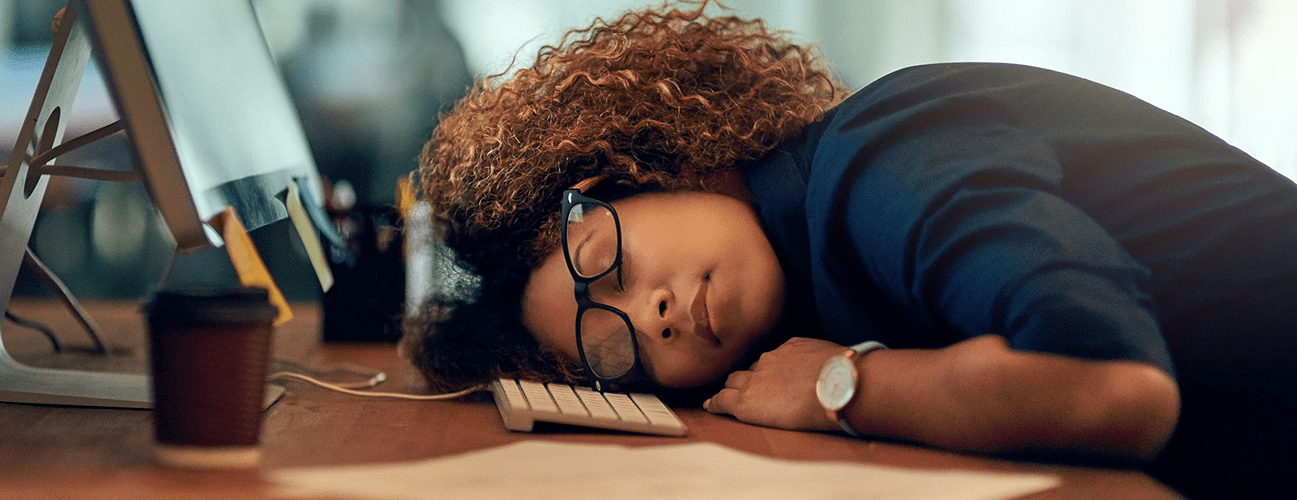
Symptom #12 – Profound Fatigue or Weakness That Won’t Go Away
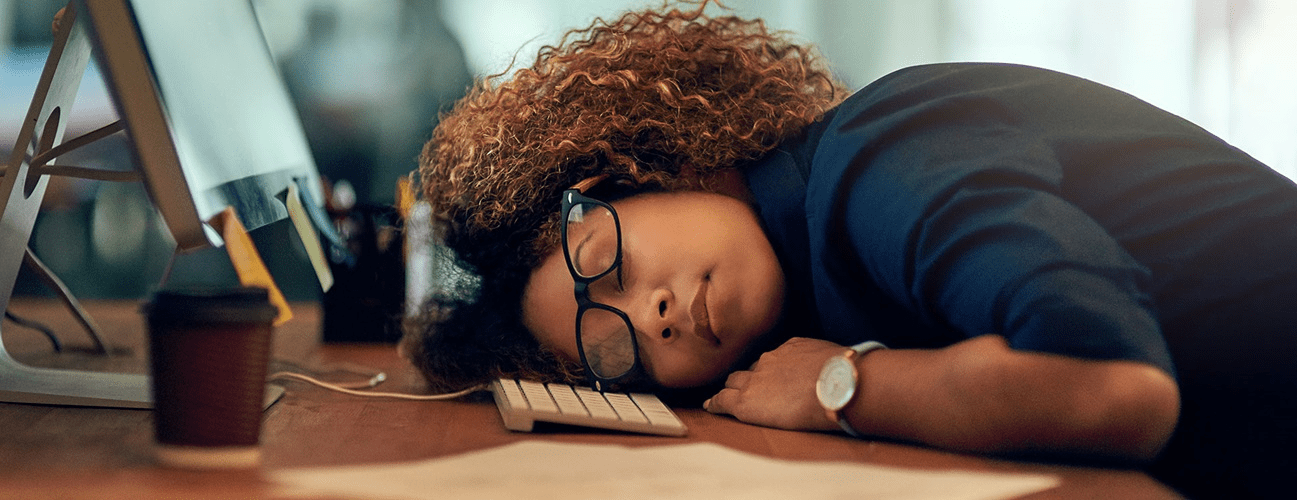
Imagine Lisa, 62, who used to hike weekends but now feels exhausted after simple chores. Rest doesn’t help; it’s a deep, draining tiredness unrelated to activity.
Research from the American Cancer Society notes fatigue as a common early complaint. Chronic inflammation and the body’s fight against cancer sap energy reserves. You might think, “I’m just getting older.” But if it’s unrelenting and new, it deserves attention.
This often pairs with other signs. The next one hits your weight unexpectedly.
Symptom #11 – Unexplained Weight Loss Without Diet or Exercise Changes
Think of Mark, 58, dropping 15 pounds in months despite eating normally. Clothes hang loose; appetite fades subtly.
Unintentional weight loss ranks among the most frequent symptoms, per Mayo Clinic reports. Cancer cells consume energy voraciously, and poor nutrient absorption from pancreatic issues worsens it. Many dismiss it as “good metabolism returning.”
But combined with fatigue? It raises red flags. Digestive troubles often follow.
Symptom #10 – Loss of Appetite or Feeling Full Quickly
Envision sitting down to a favorite meal, but eating just a few bites leaves you stuffed—or worse, nauseous at the thought of food.
The pancreas aids digestion; tumors disrupt enzyme production, leading to early satiety or disinterest in eating. Cleveland Clinic highlights this as a key digestive sign.
You may wonder if it’s acid reflux. If persistent, track it. Pain lurks nearby.
- Quick Self-Check: Meals feel burdensome; you skip them; portions shrink dramatically.
- Why It Matters: Leads to malnutrition; compounds weight loss.
- Early Tip: Note patterns; share with your doctor.
Symptom #9 – Upper Abdominal Pain That Radiates to the Back
Recall John, 65, feeling a dull ache in his upper belly after eating, worsening when lying down and easing when leaning forward.
Pain often starts mild in the abdomen and spreads to the mid-back. Tumors press on nerves or organs, per multiple sources.
“But it’s just indigestion,” many say. If constant or worsening, don’t delay. Jaundice might appear next.
Symptom #8 – Jaundice: Yellowing of Skin or Eyes
Picture noticing your skin or the whites of your eyes turning yellowish, almost like a bruise that won’t fade.
Jaundice tops lists when tumors block the bile duct (common in head-of-pancreas cancers). Mayo Clinic describes it as a classic sign, often with itching.
This can lead to earlier detection in some cases. But watch the urine and stools too.
Symptom #7 – Dark Urine and Pale or Greasy Stools
Think of urine turning cola-dark while stools become light, clay-colored, or floaty and foul-smelling.
Bile blockage causes these changes. American Cancer Society links them directly to jaundice.
Greasy stools signal fat malabsorption from lacking pancreatic enzymes. Alarming? Yes—see a doctor quickly.
| Symptom Group | Key Examples | Potential Reason |
|---|---|---|
| Digestive | Appetite loss, nausea, greasy stools | Enzyme disruption, blockage |
| Pain & Fatigue | Abdominal/back pain, exhaustion | Tumor pressure, inflammation |
| Visible Changes | Jaundice, dark urine, pale stools | Bile duct obstruction |
This table shows how symptoms cluster—spotting multiples heightens concern.
Symptom #6 – New-Onset Diabetes or Sudden Blood Sugar Changes
Visualize being diagnosed with diabetes out of nowhere, especially after 50, or existing diabetes becoming hard to control.
Pancreatic tumors can impair insulin production. Mayo Clinic flags new diabetes with weight loss or jaundice as suspicious.
“But diabetes runs in my family.” True, but abrupt onset without clear cause needs checking.
Nausea often joins in.
Symptom #5 – Nausea, Vomiting, or Indigestion
Envision frequent queasiness, occasional vomiting, or ongoing heartburn-like discomfort.
Tumors obstruct digestion or press on the stomach. Cleveland Clinic includes these in common complaints.
Many blame diet or meds. Persistence changes the story.
Symptom #4 – Bloating or Abdominal Swelling
Feel your belly distended or gassy more often, even without big meals.
Digestive slowdown causes buildup. Pancreatic Cancer Action Network notes bloating as underreported.
“But it’s IBS.” If new and unexplained, investigate further.
Symptom #3 – Itchy Skin (Often with Jaundice)
Imagine relentless itching, especially on palms or soles, driving you mad.
Bile salts build up in skin from blockage. This accompanies jaundice frequently.
Scratching offers no relief. It’s a body alarm.
Symptom #2 – Blood Clots, Especially in Legs or Lungs
Think of sudden leg swelling, pain, or breathing issues from clots.
Cancer increases clotting risk. American Cancer Society lists this as notable.
Unexplained clots? Seek urgent care.
Symptom #1 – Enlarged Gallbladder or Liver (Detected by Exam)
In some, doctors feel an enlarged gallbladder during checkups—no pain, but abnormal.
Tumor blockage causes this. It’s a clinical sign urging imaging.
This often ties to jaundice and signals need for fast evaluation—these could truly impact outcomes.
What to Do If You Recognize These Signs: Next Safe Steps
Track symptoms: Duration, severity, combinations. Journal them.
See your doctor promptly—start with primary care; they may refer to gastroenterology or oncology.
Tests could include blood work, imaging (CT/MRI), or endoscopic ultrasound. Early action improves options.
Worried it’s “nothing”? Better safe. Many symptoms mimic benign issues, but ruling out serious ones brings relief.
| Action Step | How to Begin | Important Reminder |
|---|---|---|
| Symptom Log | Daily notes on changes | Helps doctors spot patterns |
| Doctor Visit | Describe all symptoms | Mention persistence/combos |
| Lifestyle Support | Stay hydrated; eat small meals | While awaiting evaluation |
This guide promotes proactive, calm steps.
- Supportive Habits: Hydrate often; choose easy-to-digest foods; avoid alcohol/smoking.
- Monitoring: Watch for worsening pain, severe jaundice, breathing issues.
- Common Errors to Avoid: Dismissing as age-related; delaying checks; self-diagnosing.
Act on These Signs Before It’s Too Late
Pancreatic cancer’s low survival rate—around 13% at five years—stems largely from late detection. Recap: unexplained weight loss, persistent pain, jaundice, new diabetes, fatigue—these shock people when linked.
You can shift odds by listening to your body. If any resonate, contact a healthcare provider today. Early insight often leads to better management.
P.S. Awareness grows hope—pancreatic cancer research advances yearly. Share this with loved ones; one conversation could change everything.
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.