Imagine sipping your morning coffee when a sudden wave of dizziness hits, making the room spin like a carousel. Or noticing your words slurring mid-conversation, brushing it off as tiredness. What if these fleeting moments were your body’s urgent whispers? Picture the sharp throb of an unfamiliar headache, or a brief numbness tingling in your arm. You’re about to uncover 10 potential early indicators that research links to increased stroke risk weeks ahead. But first, why do these subtle signals often go unnoticed?
Strokes can strike without warning, but many people experience hints in the preceding weeks. Studies suggest transient ischemic attacks (TIAs), or “mini-strokes,” occur before about 15% of full strokes, often within days or weeks. Have you felt unexplained fatigue dragging you down lately?
The issue? These signs mimic everyday ailments, leading many over 45 to dismiss them. Yet, ignoring them might heighten risks. Emerging insights point to prodromal symptoms that could appear intermittently up to a month prior.
And the unbelievable part? Your body might be signaling distress long before a major event. Ready to explore? Let’s countdown 10 potential warning signs, each with real-life resonance.
The Hidden Truth About Pre-Stroke Signals
Meet Robert, a 62-year-old retiree from California. He chalked up his recurring dizziness to aging, until a major stroke changed everything. Afterward, he realized those spins were clues.
Similar stories abound. While classic symptoms hit suddenly, subtler ones may build. But the countdown reveals more. What’s the least expected first?
10. Persistent Unusual Fatigue
Envision dragging through days, that bone-deep exhaustion no nap fixes. Some reports link extreme tiredness to reduced brain blood flow weeks prior.
You might think, “Just stress?” But if unexplained, it warrants attention. This subtle drain sets the stage for more noticeable shifts.
9. Frequent Dizziness or Balance Issues
Picture standing up, the world tilting unexpectedly, like seasickness on dry land. Sudden dizziness may signal circulation glitches.

Research notes this in pre-stroke phases, often fleeting. Feel that unsteady wobble? It could be key. But wait, headaches intensify next.
8. Severe or Unusual Headaches
Recall a thunderclap headache, sharp and unrelenting, unlike your usual ones. Sudden severe headaches top lists of potential alerts.
Sources describe them as “worst ever,” possibly from vessel strain. That pounding intensity? Unbelievable, yet telling.
You’re wondering, “Migraine?” Differentiation matters. Vision changes surprise ahead.
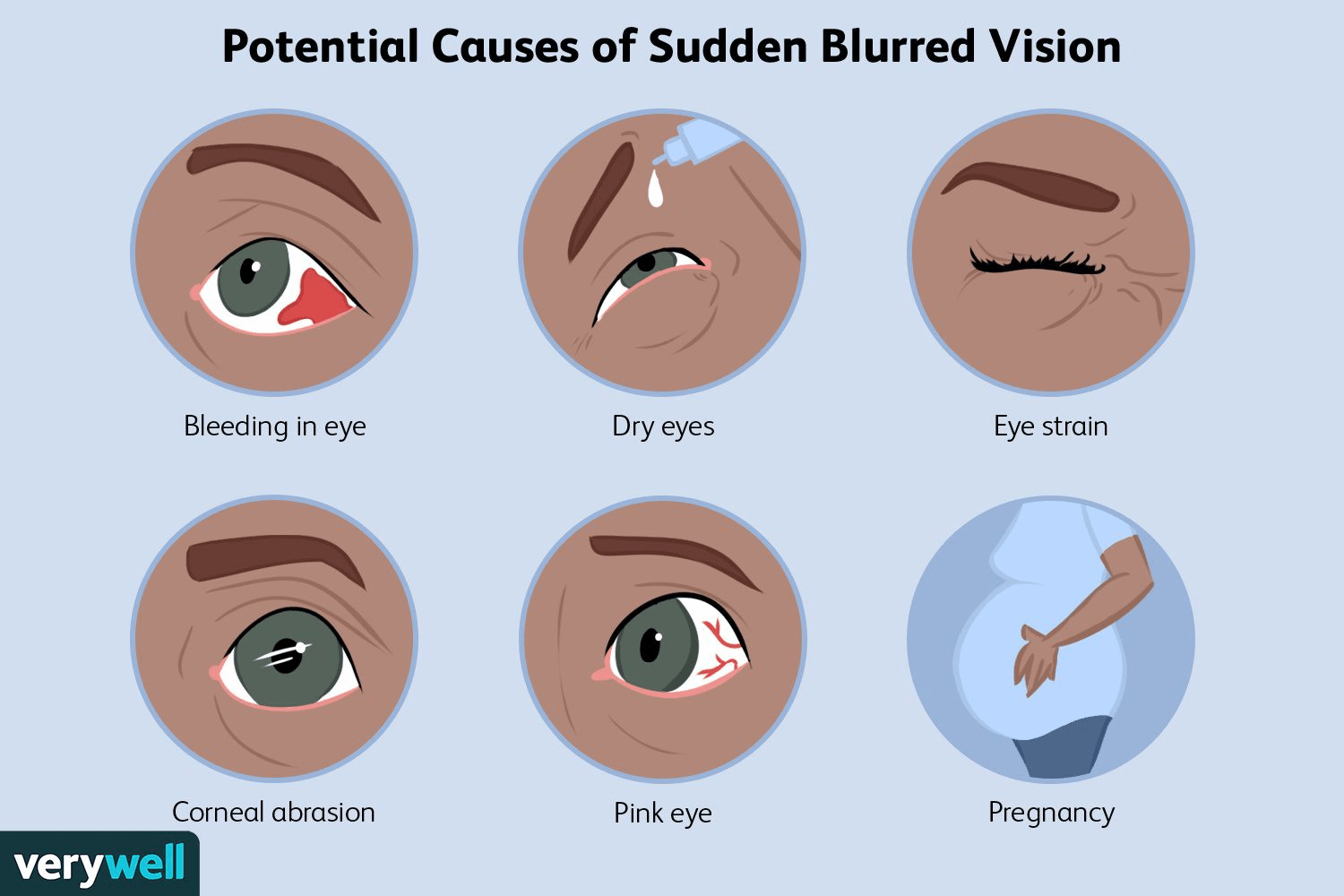
7. Sudden Vision Problems
Imagine blurred sight in one eye, like fog rolling in abruptly, clearing later. Partial loss or double vision may hint at issues.
This intermittent blur affects many pre-event. See those flashing lights? Don’t ignore.
But hold on, numbness escalates.
6. Intermittent Numbness or Weakness
Think of your arm going tingly numb briefly, strength returning soon. One-sided weakness, even temporary, raises flags.
Often on face, arm, or leg—classic, yet early versions come and go. Feel that pins-and-needles fade?
5. Brief Episodes of Confusion
Visualize struggling to follow a conversation, mind foggy momentarily. Sudden confusion or memory lapses may emerge.
This mental haze, though short, signals potential. Ever lost your train of thought oddly?
Speech difficulties shock next.
4. Temporary Speech Difficulties
Envision words slurring unexpectedly, or trouble finding them, resolving quickly. Slurred speech in bursts is a core clue.
Many experience this pre-stroke. That garbled moment? Alarming.
3. Short-Lived Coordination Problems
Picture dropping items clumsily, balance off for minutes. Walking unsteadily briefly may indicate.
This transient waver ties to brain signals. Feel off-kilter suddenly?
Vision ties in deeper.
2. Blurred or Lost Vision in One Eye
Recall darkness in one eye momentarily, like a curtain falling. Amaurosis fugax, temporary blindness, warns strongly.
This unbelievable blackout often precedes. See clearly again? Still serious.
1. Transient Ischemic Attack (TIA) Episodes
The ultimate reveal: Full mini-stroke symptoms resolving fast. TIA mimics stroke but passes—yet signals high risk soon.
Research shows many strokes follow within days or weeks. This game-changer demands immediate action.
How do classic signs compare?
| Sign | Timing | Potential Indication |
|---|---|---|
| Fatigue | Weeks prior | Reduced flow |
| Dizziness | Intermittent | Balance disruption |
| Headache | Sudden severe | Vessel pressure |
| Vision blur | Brief episodes | Eye blood supply |
| Numbness | One-sided transient | Weakness onset |
| Confusion | Short fog | Mental processing |
| Speech slur | Temporary | Language areas |
| Coordination | Fleeting | Motor control |
| Blurred eye | Curtain-like | Carotid issue |
| TIA | Full but resolves | Imminent risk |
This overview spotlights patterns. Ready to act safely?
Recognizing and Responding Promptly
Consider Linda, a 55-year-old teacher from New York. Her brief slurred speech episodes led to checks—preventing worse.
Start by knowing FAST: Face droop, Arm weakness, Speech, Time to call 911.
Any suspicious sign? Seek evaluation urgently. You might think, “It went away.” Still critical.
| Action | When | Why |
|---|---|---|
| Note symptoms | Immediately | Track onset |
| Call provider | Persistent or recurrent | Risk assessment |
| Emergency if sudden | Any time | Possible active event |
| Lifestyle check | Ongoing | Manage risks like BP |
This stresses vigilance. What if spotting one changes outcomes?
- Ask yourself: New fatigue lately?
- Monitor: Track unusual feelings.
- Discuss: Share with loved ones.
These steps empower. Evidence emphasizes early intervention.
Don’t risk missing these whispers. Recap top three: TIA episodes, one-eye vision loss, severe headaches.
Act now—your future vitality awaits.
P.S. Surprisingly, controlling blood pressure may slash risks dramatically. Share this—save a life.
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.